Volume 29, Issue 3 (10-2020)
JGUMS 2020, 29(3): 22-33 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mozaffari M, Mehrinejad S A, Peyvstegar M, Soltani S. Compared Injury Brain Traumatic Severe With Men in Impairment Cognitive Men Healthy to. JGUMS 2020; 29 (3) :22-33
URL: http://journal.gums.ac.ir/article-1-2232-en.html
URL: http://journal.gums.ac.ir/article-1-2232-en.html
1- Department of Psychology, Faculty of Education and Psychology, Alzahra University, Tehran, Iran., Tehran, Faculty of Psychology and Educational Sciences, Alzahra University
2- Department of Psychology, Faculty of Education and Psychology, Alzahra University, Tehran, Iran.
3- Department of Forensic Medicine, School of Medicine, Iran University of Medical Science, Tehran, Iran., Shohadaye Haftome Tir Hospital
2- Department of Psychology, Faculty of Education and Psychology, Alzahra University, Tehran, Iran.
3- Department of Forensic Medicine, School of Medicine, Iran University of Medical Science, Tehran, Iran., Shohadaye Haftome Tir Hospital
Full-Text [PDF 3862 kb]
(1177 Downloads)
| Abstract (HTML) (2883 Views)
Full-Text: (2869 Views)
1. Introduction
ne of the most common cognitive problems after traumatic brain injury is impaired executive function. The recovery after traumatic brain injury takes place one year after injury; after this period, the brain injured patient faces an uncertain future. In some patients, improvement is observed even 5-10 years after injury, while in some patients the injury is worsened [7]. It is associated with cognitive dysfunction as a result of impaired information processing, memory, attention, planning, and executive function. The aim of this study was to evaluate cognitive impairment in men with a history of Severe Traumatic Brain Injury (STBI) compared to healthy men.
2. Materials and Methods
This causal-comparative study (Ethical approval code: IR.UT.PSYEDU.REC.1398.004) was conducted from February 2017 to July 2019 on two groups of individuals; 20 male patients aged 30-55 years having STBI in the past one year and admitted to the intensive care units of two Shohaday-e-Haftom-e-Tir and Baqiyatallah hospitals, in Tehran, Iran, and 64 healthy men that had met all inclusion criteria (age of 30-55 years, no addiction to drugs and alcohol use, no other concurrent diseases, educational level ranging from first grade middle-school education to associate degree). After explaining the study method and Objectives to participants and obtaining a written informed consent from them, their demographic characteristics were recorded via interview, and then they underwent the Wisconsin Card Sorting Test (WCST) which was taken by a clinical psychologist. This test a reliable tool for assessment of cognitive impairment in adults and can measure concept formation and reasoning abilities. The professional manual for the WCST was written by Heaton et al. [32]. It has been found to be sensitive to frontal-lobe dysfunction, providing a clinical measure of abstract thinking and the ability to shift cognitive sets. Inter-rater reliability of this test ranges from 0.91 to 0.96 and its generalizability coefficients ranges from 0.39 to 0.72. The average concurrent validity regarding the agreement between this test and other measures of concept formation is 0.83. The Cronbach’s alpha of WCST showed has accepatable reliability in Iranian samples. The WCST responses were compared between the two study groups regarding the presentation of cards and the presentation of feedback signals. Data were analyzed in SPSS V. 21 software using Mean and Standard Deviation (SD) and ANOVA.
3. Results
The Mean±SD age of STBI patients and healthy men was 40.10±9.61 and 41.81±8.60 years, respectively; most of them (35.7%) had 35-30 years of age, while minority of them (11.9%) were at an age range of 41-45 and 46-50 years. Most of them (34.5%) had first-grade to third-grade high school education, while minority of them (7.1%) had associate degree. The overall WCST score was lower in patients than in healthy men. The mean number of categories completed in patients (1.00) was lower than in healthy subjects (2.47), and there was a significant difference between patients and healthy men (P<0.01). Descriptive statistics of WCST scores for the men with and without STBI are presented in Table 1.
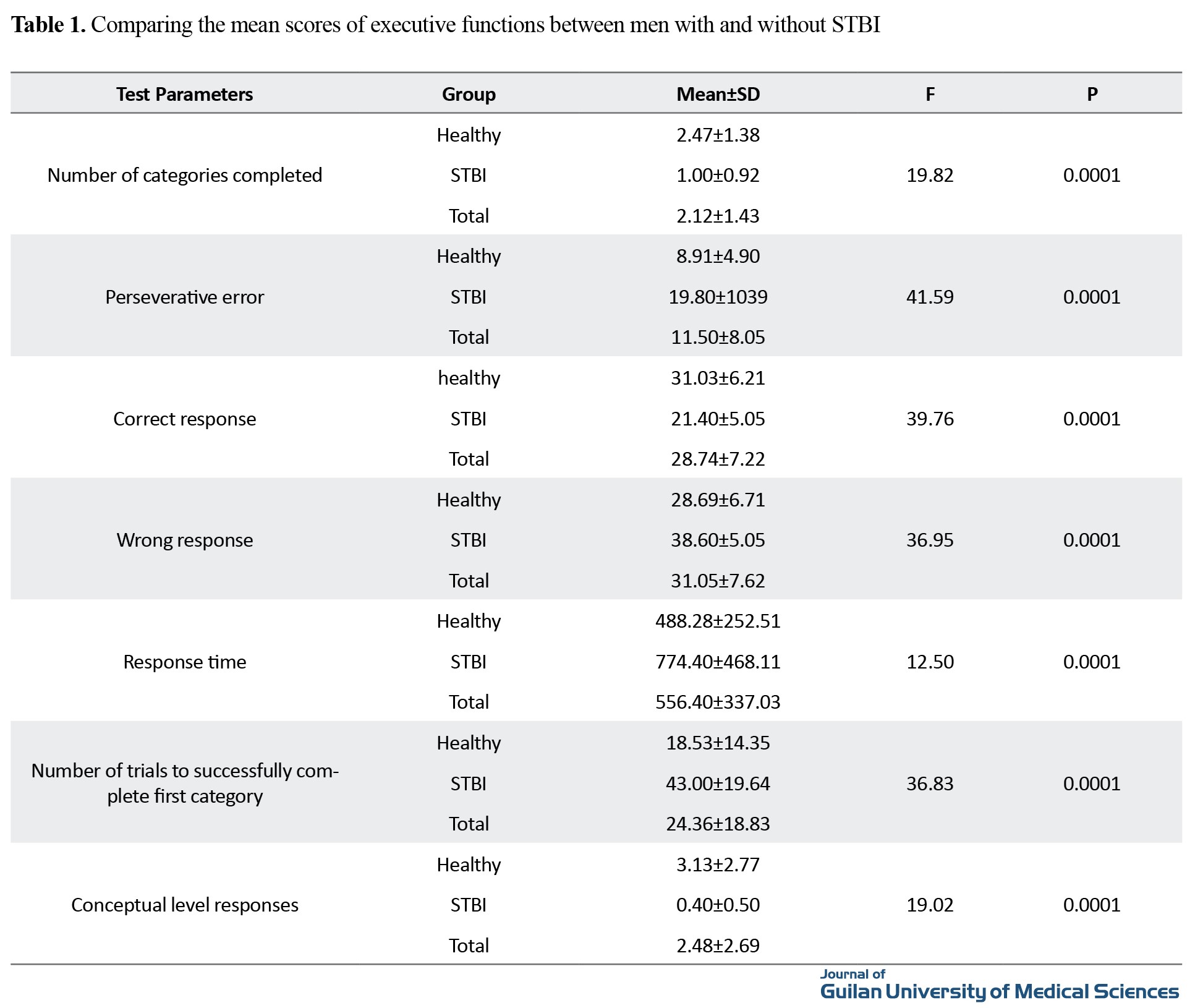
The results showed that the correct responses, response time, number of trials to successfully complete first category, and conceptual level responses were lower in patients with STBI than in healthy subjects, and patients had more perseverative errors than healthy subjects. Patients had a mean correct response of 21.40±5.05, while for the healthy group it was 31.03±6.21 (Table 1).
ANOVA was used to determine whether there were any statistically significant differences in the executive functions between the two groups. The results showed a significant difference between two groups in the number of categories completed (F(1,112)=19.82, P<0.001), perseverative errors (F(1,82)=41.59, P<0.001), correct response (F(1,82)=39.76, P<0.001), wrong responses (F(1,82)=36.95, P<0.001), response time (F(1,82)=12.50, P<0.001), number of trials to successfully complete first category (F(1,82)=36.83, P<0.001), and conceptual level responses (F(1,82)=19.02, P<0.001).
4. Conclusion
There was a significant difference between men with STBI and healthy ones in the executive functions. STBI can cause different psychological consequences, including impaired functions in Orbitofrontal Cortex (OFC) [24]. Impairments in memory, attention, executive functions, and behavioral control followed by injury to the frontal and temporal lobes, are particularly troublesome [13]. Studies have suggested that OFC acts as a critical frontal brain area that informs the downstream regions about the need to suppress the behavior. Evidence for this arose when damage to OFC was shown to promote disinhibition operationalized as perseveration during extinction tasks. Many of these studies suggest that OFC provides a type of inhibitory signal that dampens behavioral responding when such control is necessary for accurate performance. Study of the patients with STBI can increase our knowledge of STBI, and help improve its treatment and increase rehabilitation efforts.
Ethical Considerations
Compliance with ethical guidelines
This study ethically approved by Alzahra University, Tehran, (Code: IR.UT.PSYEDU.REC.1398.004).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, writing: Mohaddeseh Mozaffari, Mehrangiz Peyvstegar; Methodology: Mehrangiz Peyvstegar, Mohaddeseh Mozaffari, Siamak Soltani; Investigation: Mehrangiz Peyvstegar, Mohaddeseh Mozaffari, Seyed Abolghasem Mehrinejad; Editing: Seyed Abolghasem Mehrinejad, Siamak Soltani; Resorrces, funding, acquisition: All author; Supervision: Mehrangiz Peyvstegar, Mohaddeseh Mozaffari, Seyed Abolghasem Mehrinejad.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would link to thank all supervisors and staff of Shohaday-e-Haftom-e-Tir and Baqiyatallah Hospitals, and also would link to thank all STBI patients fot thei cooperation.
References
ne of the most common cognitive problems after traumatic brain injury is impaired executive function. The recovery after traumatic brain injury takes place one year after injury; after this period, the brain injured patient faces an uncertain future. In some patients, improvement is observed even 5-10 years after injury, while in some patients the injury is worsened [7]. It is associated with cognitive dysfunction as a result of impaired information processing, memory, attention, planning, and executive function. The aim of this study was to evaluate cognitive impairment in men with a history of Severe Traumatic Brain Injury (STBI) compared to healthy men.
2. Materials and Methods
This causal-comparative study (Ethical approval code: IR.UT.PSYEDU.REC.1398.004) was conducted from February 2017 to July 2019 on two groups of individuals; 20 male patients aged 30-55 years having STBI in the past one year and admitted to the intensive care units of two Shohaday-e-Haftom-e-Tir and Baqiyatallah hospitals, in Tehran, Iran, and 64 healthy men that had met all inclusion criteria (age of 30-55 years, no addiction to drugs and alcohol use, no other concurrent diseases, educational level ranging from first grade middle-school education to associate degree). After explaining the study method and Objectives to participants and obtaining a written informed consent from them, their demographic characteristics were recorded via interview, and then they underwent the Wisconsin Card Sorting Test (WCST) which was taken by a clinical psychologist. This test a reliable tool for assessment of cognitive impairment in adults and can measure concept formation and reasoning abilities. The professional manual for the WCST was written by Heaton et al. [32]. It has been found to be sensitive to frontal-lobe dysfunction, providing a clinical measure of abstract thinking and the ability to shift cognitive sets. Inter-rater reliability of this test ranges from 0.91 to 0.96 and its generalizability coefficients ranges from 0.39 to 0.72. The average concurrent validity regarding the agreement between this test and other measures of concept formation is 0.83. The Cronbach’s alpha of WCST showed has accepatable reliability in Iranian samples. The WCST responses were compared between the two study groups regarding the presentation of cards and the presentation of feedback signals. Data were analyzed in SPSS V. 21 software using Mean and Standard Deviation (SD) and ANOVA.
3. Results
The Mean±SD age of STBI patients and healthy men was 40.10±9.61 and 41.81±8.60 years, respectively; most of them (35.7%) had 35-30 years of age, while minority of them (11.9%) were at an age range of 41-45 and 46-50 years. Most of them (34.5%) had first-grade to third-grade high school education, while minority of them (7.1%) had associate degree. The overall WCST score was lower in patients than in healthy men. The mean number of categories completed in patients (1.00) was lower than in healthy subjects (2.47), and there was a significant difference between patients and healthy men (P<0.01). Descriptive statistics of WCST scores for the men with and without STBI are presented in Table 1.
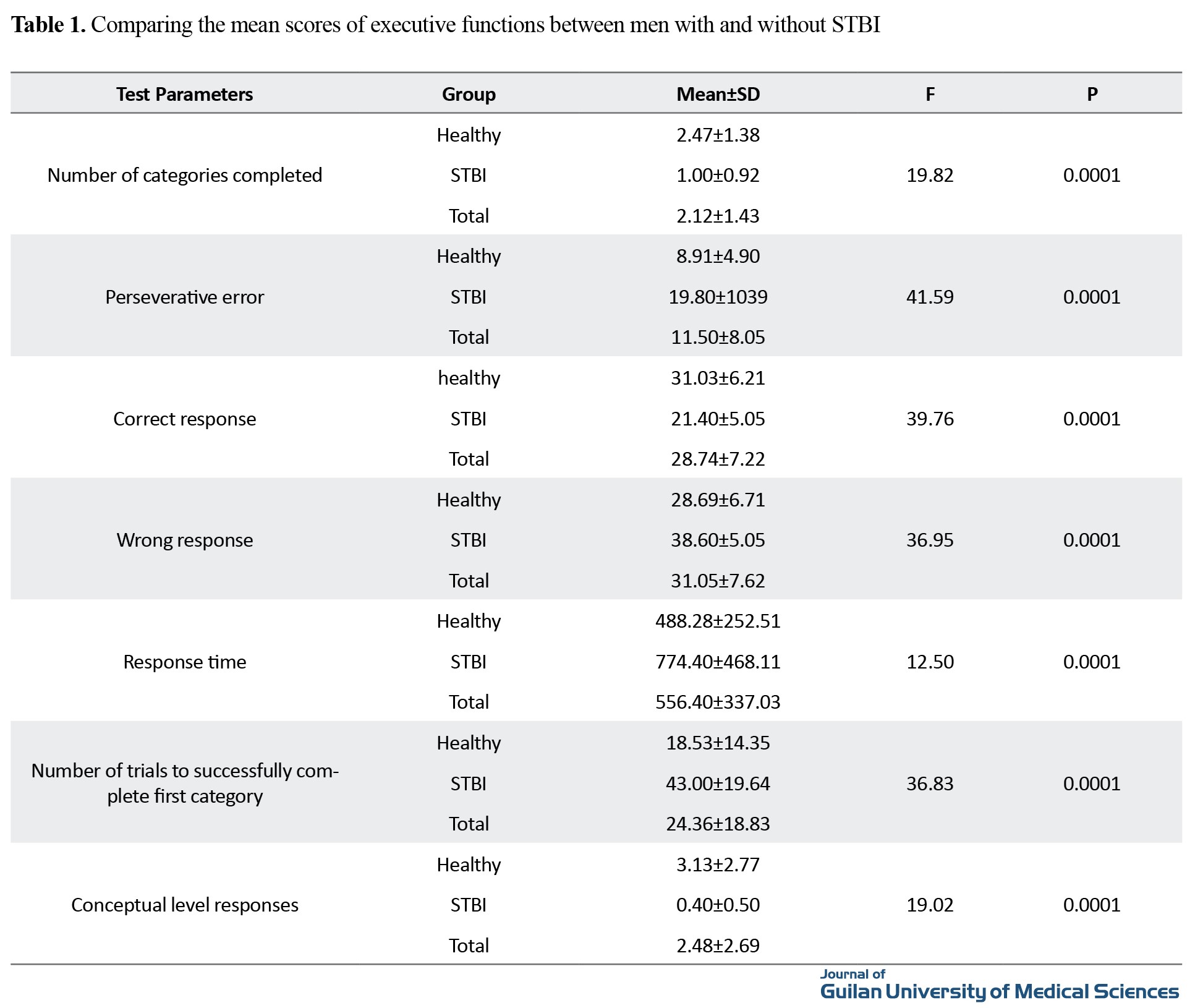
The results showed that the correct responses, response time, number of trials to successfully complete first category, and conceptual level responses were lower in patients with STBI than in healthy subjects, and patients had more perseverative errors than healthy subjects. Patients had a mean correct response of 21.40±5.05, while for the healthy group it was 31.03±6.21 (Table 1).
ANOVA was used to determine whether there were any statistically significant differences in the executive functions between the two groups. The results showed a significant difference between two groups in the number of categories completed (F(1,112)=19.82, P<0.001), perseverative errors (F(1,82)=41.59, P<0.001), correct response (F(1,82)=39.76, P<0.001), wrong responses (F(1,82)=36.95, P<0.001), response time (F(1,82)=12.50, P<0.001), number of trials to successfully complete first category (F(1,82)=36.83, P<0.001), and conceptual level responses (F(1,82)=19.02, P<0.001).
4. Conclusion
There was a significant difference between men with STBI and healthy ones in the executive functions. STBI can cause different psychological consequences, including impaired functions in Orbitofrontal Cortex (OFC) [24]. Impairments in memory, attention, executive functions, and behavioral control followed by injury to the frontal and temporal lobes, are particularly troublesome [13]. Studies have suggested that OFC acts as a critical frontal brain area that informs the downstream regions about the need to suppress the behavior. Evidence for this arose when damage to OFC was shown to promote disinhibition operationalized as perseveration during extinction tasks. Many of these studies suggest that OFC provides a type of inhibitory signal that dampens behavioral responding when such control is necessary for accurate performance. Study of the patients with STBI can increase our knowledge of STBI, and help improve its treatment and increase rehabilitation efforts.
Ethical Considerations
Compliance with ethical guidelines
This study ethically approved by Alzahra University, Tehran, (Code: IR.UT.PSYEDU.REC.1398.004).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, writing: Mohaddeseh Mozaffari, Mehrangiz Peyvstegar; Methodology: Mehrangiz Peyvstegar, Mohaddeseh Mozaffari, Siamak Soltani; Investigation: Mehrangiz Peyvstegar, Mohaddeseh Mozaffari, Seyed Abolghasem Mehrinejad; Editing: Seyed Abolghasem Mehrinejad, Siamak Soltani; Resorrces, funding, acquisition: All author; Supervision: Mehrangiz Peyvstegar, Mohaddeseh Mozaffari, Seyed Abolghasem Mehrinejad.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would link to thank all supervisors and staff of Shohaday-e-Haftom-e-Tir and Baqiyatallah Hospitals, and also would link to thank all STBI patients fot thei cooperation.
References
- Mangia AL. [Cognitive assessment and rehabilitation of subjects with traumatic brain injury (Italian)]. [PhD. dissertation]. Bologna: Università di Bologna; 2015. http://amsdottorato.unibo.it/7063/1/Tesi_Con_Frontespizio.pdf
- Muelbl MJ, Slaker ML, Shah AS, Nawarawong NN, Gerndt CH, Budde MD, et al. Effects of mild blast traumatic brain injury on cognitive-and addiction-related behaviors. Scientific reports. 2018; 8(1):9941. [DOI:10.1038/s41598-018-28062-0] [PMID] [PMCID]
- Arnould A, Rochat L, Dromer E, Azouvi P, Van der Linden M. Does multitasking mediate the relationships between episodic memory, attention, executive functions and apathetic manifestations in traumatic brain injury? Journal of neuropsychology. 2018; 12(1):101-19. [DOI:10.1111/jnp.12107] [PMID]
- Hanks R, Millis S, Scott S, Gattu R, O’Hara NB, Haacke M, et al. The relation between cognitive dysfunction and diffusion tensor imaging parameters in traumatic brain injury. Brain injury. 2019; 33(3):355-63. [DOI:10.1080/02699052.2018.1553073] [PMID]
- Vasquez BP, Tomaszczyk JC, Sharma B, Colella B, Green REA. Longitudinal recovery of executive control functions after moderate-severe traumatic brain injury: examining trajectories of variability and ex-Gaussian parameters. Neurorehabilitation and neural repair. 2018; 32(3):191-9. [DOI:10.1177/1545968318760727] [PMID]
- Molteni E, Pagani E, Strazzer S, Arrigoni F, Beretta E, Boffa G, et al. Fronto-temporal vulnerability to disconnection in paediatric moderate and severe traumatic brain injury. European journal of neurology. 2019; 26(9):1183-90. [DOI:10.1111/ene.13963] [PMID]
- Lesimple B, Caron E, Lefort M, Debarle C, Pélégrini-Issac M, Cassereau D, et al. Long-term cognitive disability after traumatic brain injury: Contribution of the DEX relative questionnaires. Neuropsychological Rehabilitation. 2020; 30(10):1905-24. [DOI:10.1080/09602011.2019.1618345] [PMID]
- Keelan RE, Mahoney EJ, Sherer M, Hart T, Giacino J, Bodien YG, et al. Neuropsychological Characteristics of the confusional state following traumatic brain injury. Journal of the International Neuropsychological Society. 2019; 25(3):302-13. [DOI:10.1017/S1355617718001157] [PMID]
- Owens JA, Spitz G, Ponsford JL, Dymowski AR, Willmott C. An investiga tion of white matter integrity and attention deficits following traumatic brain injury. Brain injury. 2018; 32(6):776-83. [DOI:10.1080/02699052.2018.1451656] [PMID]
- Kozak KM. Mild Traumatic Brain Injuries and Their Implications on Changes in Event Related Potentials: A look into Visual Gating (P50). [MSc. thesis]. New York: City University of New York; 2018. https://academicworks.cuny.edu/cc_etds_theses/728/
- Marschner L, Schreurs A, Lechat B, Mogensen J, Roebroek A, Ahmed T, et al. Single mild traumatic brain injury results in transiently impaired spatial long-term memory and altered search strategies. Behavioural brain research. 2019; 365:222-30. [DOI:10.1016/j.bbr.2018.02.040] [PMID]
- Bangirana P, Giordani B, Kobusingye O, Murungyi L, Mock C, John CC, et al. Patterns of traumatic brain injury and six-month neuropsychological outcomes in Uganda. BMC neurology. 2019; 19(1):18. [DOI:10.1186/s12883-019-1246-1] [PMID] [PMCID]
- McDonald S, Dalton KI, Rushby JA, Landin-Romero R. Loss of white matter connections after severe Traumatic Brain Injury (TBI) and its relationship to social cognition. Brain imaging and behavior. 2019; 13(3):819-29. [DOI:10.1007/s11682-018-9906-0] [PMID]
- Tölli A, Höybye C, Bellander BM, Borg J. Impact of pituitary dysfunction on cognitive and global outcome after traumatic brain injury and aneurysmal subarachnoid haemorrhage. Journal of rehabilitation medicine. 2019; 51(4):264-72. [DOI:10.2340/16501977-2531] [PMID]
- Hart T, Rabinowitz AR, Whyte J, Kim J. Pre-injury assessment of everyday executive function in moderate to severe traumatic brain injury. Neuropsychological rehabilitation. 2019; 29(7):1085-94. [DOI:10.1080/09602011.2017.1364271] [PMID] [PMCID]
- Chen NYC, Batchelor J. Length of post-traumatic amnesia and its prediction of neuropsychological outcome following severe to extremely severe traumatic brain injury in a litigating sample. Brain injury. 2019; 33(8):1087-96. [DOI:10.1080/02699052.2019.1610797] [PMID]
- Resch C, Anderson VA, Beauchamp MH, Crossley L, Hearps SJ, van Heugten CM, et al. Age-dependent differences in the impact of paediatric traumatic brain injury on executive functions: A prospective study using susceptibility-weighted imaging. Neuropsychologia. 2019; 124:236-45. [DOI:10.1016/j.neuropsychologia.2018.12.004] [PMID]
- Câmara-Costa H, Opatowski M, Francillette L, Toure H, Brugel D, Laurent-Vannier A, et al. Self-and parent-reported quality of Life 7 years after severe childhood traumatic brain injury in the Traumatisme Grave de l’Enfant cohort: associations with Objective and subjective factors and outcomes. Quality of life research. 2019; 29(2):515-28. [DOI:10.1007/s11136-019-02305-7] [PMID]
- Le Fur C, Câmara-Costa H, Francillette L, Opatowski M, Toure H, Brugel D, et al. Executive functions and attention 7 years after severe childhood traumatic brain injury: Results of the Traumatisme Grave de l’Enfant (TGE) cohort. Annals of Physical and Rehabilitation Medicine. 2020; 63(4):270-9. [DOI:10.1016/j.rehab.2019.09.003] [PMID]
- Svingos AM, Asken BM, Jaffee MS, Bauer RM, Heaton SC. Predicting long-term cognitive and neuropathological consequences of moderate to severe traumatic brain injury: Review and theoretical framework. Journal of clinical and experimental neuropsychology. 2019; 41(8):775-85. [DOI:10.1080/13803395.2019.1620695] [PMID]
- Fraser EE, Downing MG, Biernacki K, McKenzie DP, Ponsford JL. Cognitive reserve and age predict cognitive recovery after mild to severe traumatic brain injury. Journal of neurotrauma. 2019; 36(19):2753-61. [DOI:10.1089/neu.2019.6430] [PMID]
- Olsen A, Babikian T, Dennis EL, Ellis-Blied MU, Giza C, Marion SD, eta al. Functional brain hyperactivations are linked to an electrophysiological measure of slow interhemispheric transfer time after pediatric moderate/severe traumatic brain injury. Journal of neurotrauma. 2020; 37(2):397-409. [DOI:10.1089/neu.2019.6532] [PMID] [PMCID]
- Savulich G, Menon DK, Stamatakis EA, Pickard JD, Sahakian BJ. Personalised treatments for traumatic brain injury: cognitive, emotional and motivational targets. Psychological medicine. 2018; 48(9):1397-9 [DOI:10.1017/S0033291718000892] [PMID]
- Grandhi R, Tavakoli S, Ortega C, Simmonds MJ. A review of chronic pain and cognitive, mood, and motor dysfunction following mild traumatic brain injury: complex, comorbid, and/or overlapping conditions? Brain sciences. 2017; 7(12):160. [DOI:10.3390/brainsci7120160] [PMID] [PMCID]
- Rockswold SB, Burton PC, Chang A, McNally N, Grant A, Rockswold GL, Low WC, Eberly LE, Yacoub E, Lenglet C. Functional magnetic resonance imaging and oculomotor dysfunction in mild traumatic brain injury. Journal of neurotrauma. 2019; 36(7):1099-105. [DOI:10.1089/neu.2018.5796] [PMID] [PMCID]
- Lansdell G, Saunders B, Eriksson A, Bunn R, Baidawi S. ‘I am not drunk, I have an ABI’: findings from a qualitative study into systematic challenges in responding to people with acquired brain injuries in the justice system. Psychiatry, Psychology and Law. 2018; 25(5):737-58. [DOI:10.1080/13218719.2018.1474818] [PMID] [PMCID]
- Theadom A, Starkey N, Barker-Collo S, Jones K, Ameratunga S, Feigin V, et al. Population-based cohort study of the impacts of mild traumatic brain injury in adults four years post-injury. PLoS One. 2018; 13(1):e0191655. [DOI:10.1371/journal.pone.0191655] [PMID] [PMCID]
- Carroll LJ, Cassidy JD, Cancelliere C, Côté P, Hincapié CA, Kristman VL, et al. Systematic review of the prognosis after mild traumatic brain injury in adults: cognitive, psychiatric, and mortality outcomes: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Archives of physical medicine and rehabilitation. 2014; 95(3 Suppl):S152-73. [DOI:10.1016/j.apmr.2013.08.300] [PMID]
- Chiu EC, Wu WC, Hung JW, Tseng YH. Validity of the Wisconsin Card Sorting Test in patients with stroke. Disability and rehabilitation. 2018; 40(16):1967-71. [DOI:10.1080/09638288.2017.1323020] [PMID]
- Naderi N, Rasolian M, Yasami MT, Ashaieri H. A study of information processing and some of neuropsychological functions patient with obsessive-compulsive disorder [MA. thesis]. Tehran: Institute of Psychiatry of Tehran; 1994.
- Bergersen K, Halvorsen JØ, Tryti EA, Taylor SI, Olsen A. A systematic literature review of psychotherapeutic treatment of prolonged symptoms after mild traumatic brain injury. Brain injury. 2017; 31(3):279-89. [DOI:10.1080/02699052.2016.1255779] [PMID]
- Heaton R, Chelune G, Talley J, Kay G, Curtiss G. Wisconsin Card Sorting Test Manual: Revised and expanded. Lutz: Psychological Assessment Resources Inc, 1993. https://www.bibsonomy.org/bibtex/2db9f59c0ebfd219f28eda9773b1aa6a2/brian.mingus
Review Paper: Research |
Subject:
Special
Received: 2020/02/15 | Accepted: 2020/06/25 | Published: 2020/10/1
Received: 2020/02/15 | Accepted: 2020/06/25 | Published: 2020/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |