Volume 29, Issue 4 (1-2021)
JGUMS 2021, 29(4): 114-121 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Naghipour A, Khatirnamani Z, Kalteh E A, Taramian S. Prevalence of Tuberculosis in Diabetic Patients Living in Rural Areas of Northern Iran in 2016. JGUMS 2021; 29 (4) :114-121
URL: http://journal.gums.ac.ir/article-1-2280-en.html
URL: http://journal.gums.ac.ir/article-1-2280-en.html
1- Department of Infectious Diseases, School of Medicine, Gilan University of Medical Sciences, Rasht, Iran.
2- Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran.
3- Department of Infectious Diseases, School of Medicine, Gilan University of Medical Sciences, Rasht, Iran. , sontar2002@yahoo.com
2- Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran.
3- Department of Infectious Diseases, School of Medicine, Gilan University of Medical Sciences, Rasht, Iran. , sontar2002@yahoo.com
Full-Text [PDF 2342 kb]
(1130 Downloads)
| Abstract (HTML) (1383 Views)
Full-Text: (1935 Views)
1. Introduction
iabetes is one of the diseases that negatively affects the quality of life [1]. Diabetes is a metabolic disorder and has a direct relationship with Tuberculosis (TB) [2]. Diabetics are at higher risk for various types of infections [4, 3]. Results of a study showed that diabetes exacerbates the TB complications and affects the radiological manifestations of the disease [5]. Pulmonary infections in diabetic patients alter host defenses. Therefore, the TB severity is directly related to the blood sugar level and the host defense [3]. TB is one of the most important health challenges in the world [6] and is the leading cause of death from single infectious agent [7]. The prevalence of TB differs in different parts of world. It has been reported that 22 countries in Eastern Mediterranean as well as Pakistan, Afghanistan, Egypt, Iraq, Iran, Morocco, Somalia, Sudan, and Yemen accounted for 95% of TB cases [11, 10, 9 ,8]. According to available statistics in Iran, Sistan and Baluchestan (n=330, 16.94 per 100000 people) and Golestan (n=428, 22.88 per 100000 people) provinces have the highest TB cases [12]. Golestan Province is a TB-endemic area of Iran with the highest TB prevalence [13]. Clinical symptoms of TB are often non-specific and include fever, night sweats, weight loss, anorexia, and fatigue [14]. Various factors such as age, thoracic radiological signs, the presence of a high number of bacilli in sputum smear of patients at the beginning of treatment, diabetes, immunosuppressive drugs, irregularities in the implementation of the treatment plan, or absence from treatment session affect the success or failure of TB treatment [13, 14, 15, 16, 17, 18, 19, 20, 21].
There are differences between diabetic patients and general population in the manifestation of symptoms of various comorbidities, including TB, such as lower prevalence, cough, sputum, and weight loss [22]. Among the cities of Golestan Province, Kordkuy has the highest prevalence of diabetes (8.1%) and refractory TB cases have been observed among diabetic patients in this city. The present study aims to screen pulmonary TB and determine the prevalence of TB in people with diabetes living in rural areas of Kordkuy City.
2. Materials and Methods This is a descriptive cross-sectional study, which was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1397.219). The study population included all diabetic patients living in 19 villages of Kordkuy city. Samples were selected using a census method. The exclusion criterion was pregnancy due to not being possible to do x-ray to prevent harm to the fetus. Informed consent was obtained from all participants. Data collection was carried out using a checklist, laboratory observations, chest x-ray (except for those forbidden to radiation exposure), TB skin test, and finally collecting sputum samples from patients who were more likely to be exposed to TB. The studied variables were: Age, gender, ethnicity, smoking, use of narcotic drugs or psychotropic substances, type of diabetes, duration of diabetes, history of previous TB, history and duration of contact with TB patients, sputum smear result, lung x-ray, last fasting blood sugar level, and last HbA1C test results. The collected data were analyzed in SPSS V. 16 software.
3. Results
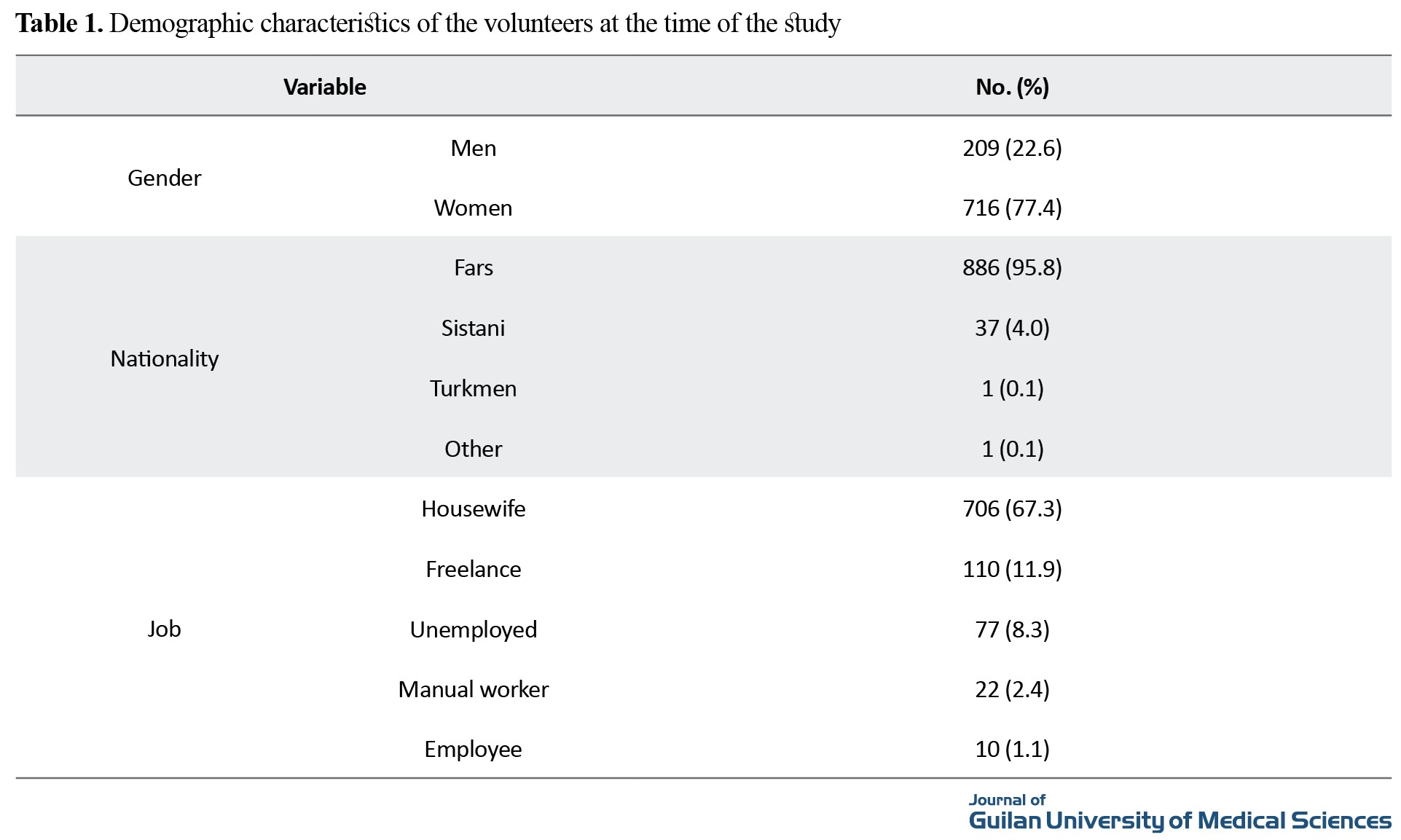
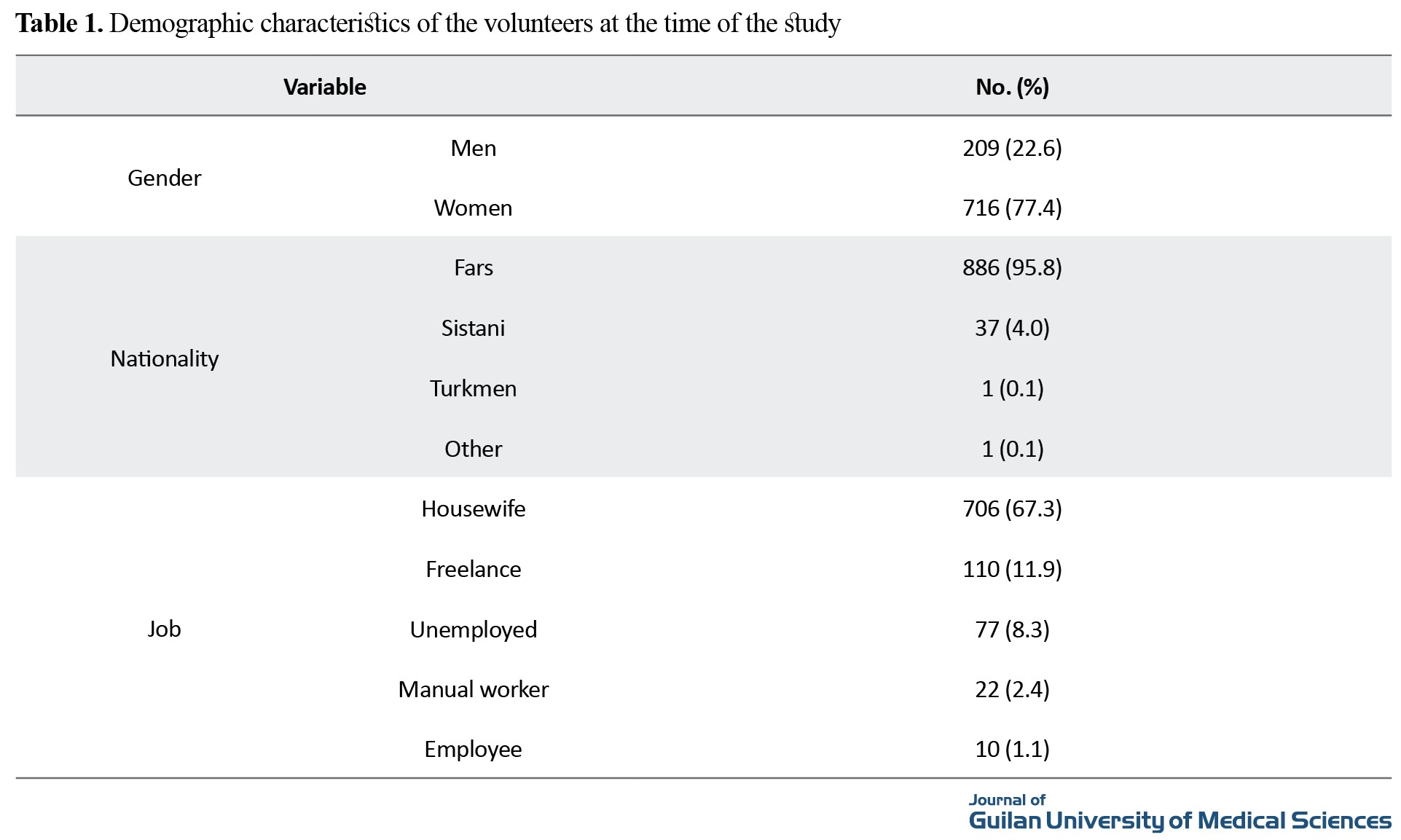
Results showed that 77.4% of participants (n=716) were female, 98.2% (n=923) were Iranian nationals, and 886 (95.8%) were Persian. Demographic characteristics of participants are shown in Table 1.
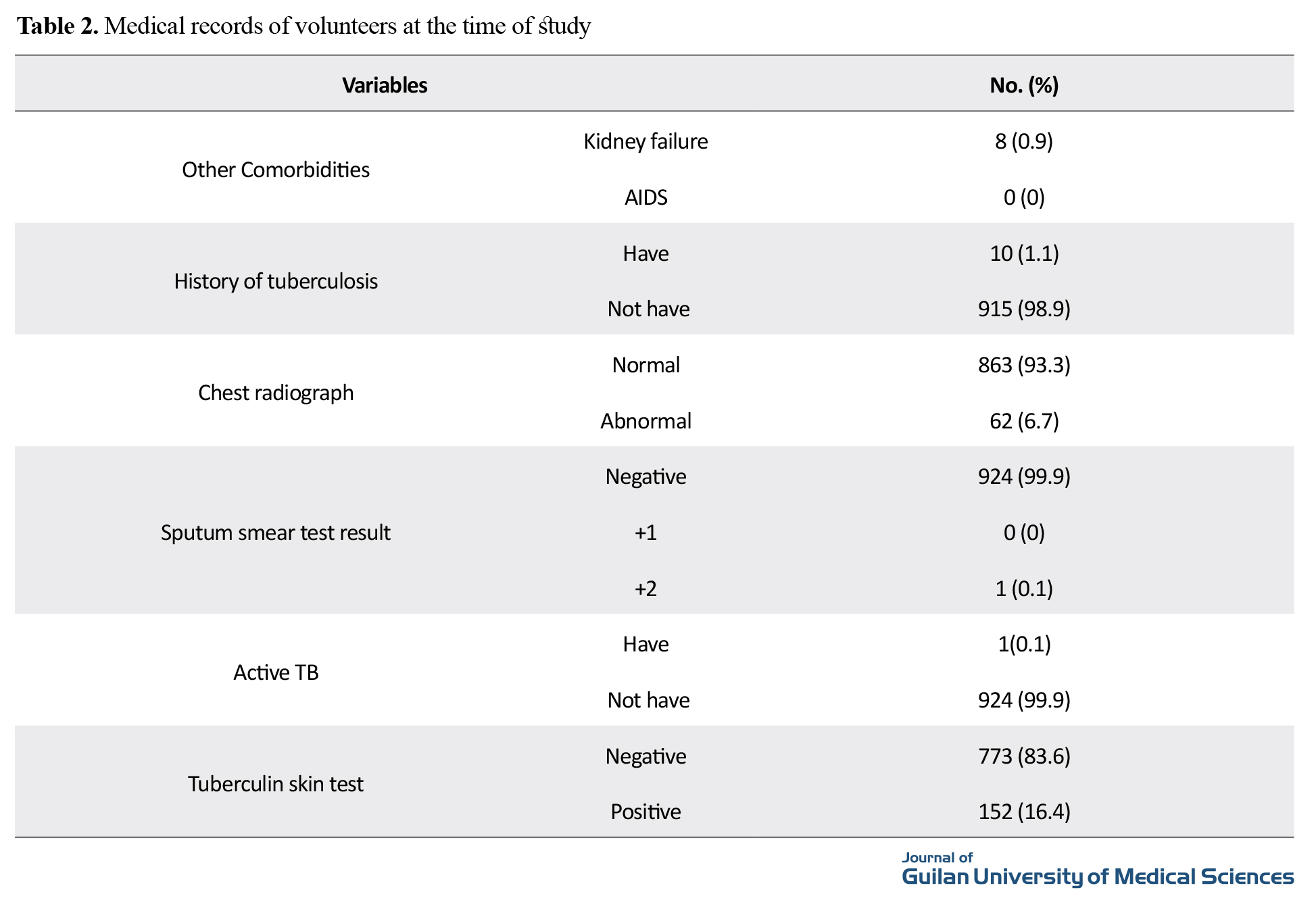
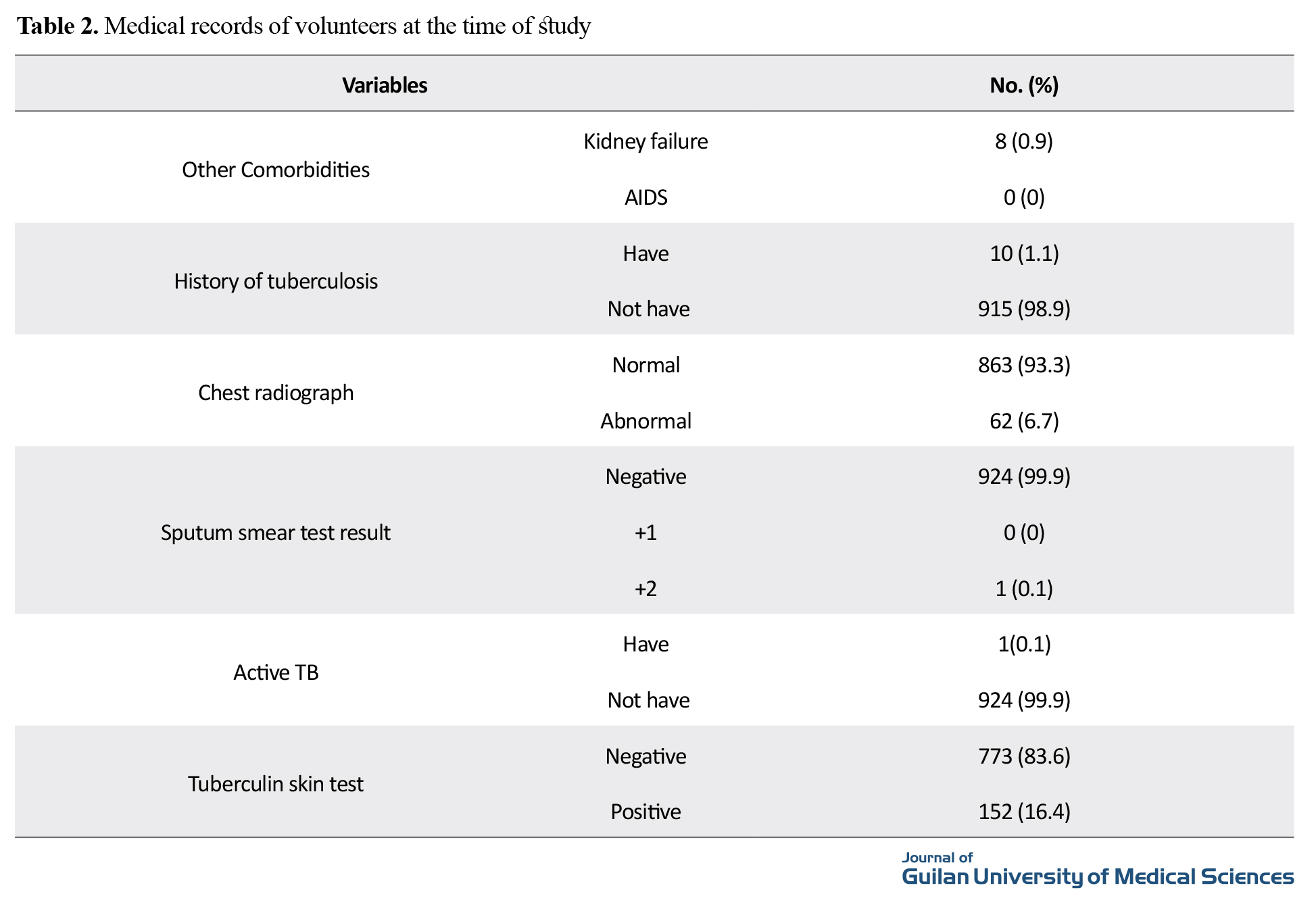
Their mean age was 58.40 ±11.10 years with a mean diabetes duration of 8.5±39.47 years. Eight patients (0.9%) had kidney failure, none had acquired immunodeficiency disease, and 10 (1.1%) had a history of TB. We identified one case of active TB with smear-positive sputum. The patient was a 55-year-old woman, housekeeper, with Persian ethnicity, one year history of diabetes, and no history of contact with TB patients (Table 2).
4. Discussion and Conclusion
Recent studies have reported the prevalence of pulmonary TB in diabetic people is 4-5 times more than that in normal people [4]. Diabetes is a risk factor with indirect role in the development of TB [17]. In a study, the incidence of TB in diabetic group was 4.7 times higher than in non-diabetic people [21]. The current study revealed the relationship between diabetes and TB and showed that the TB prevalence was about 0.001 among diabetic patients. To better compare the prevalence of the disease in the same rural population and at the same time, pulmonary TB patients living in the village but had no diabetes were also examined. Study on some diabetic patients showed that there were confounding factors that made it more difficult to diagnose the disease. For example, addiction of the TB patient and his/her spouse led to the absence of some symptoms of TB in them. There have been contradictory results about the role of TB in the development of diabetes [17, 24]. Basoglu showed no significant difference between the two groups [22].
TB prevalence among diabetic people in Kordkuy city is 60 times higher. Both TB and diabetes are health risk factors. It is also recommended to conduct large-scale clinical studies in Iran to investigate other risk factors and TB symptoms in diabetic patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Ethics Code: IR.GUMSREC.1397.219).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the officials of the centers, the volunteers, and all those who participated in the study and the efforts of Ms. Zeinab Khalilnejad.
References
iabetes is one of the diseases that negatively affects the quality of life [1]. Diabetes is a metabolic disorder and has a direct relationship with Tuberculosis (TB) [2]. Diabetics are at higher risk for various types of infections [4, 3]. Results of a study showed that diabetes exacerbates the TB complications and affects the radiological manifestations of the disease [5]. Pulmonary infections in diabetic patients alter host defenses. Therefore, the TB severity is directly related to the blood sugar level and the host defense [3]. TB is one of the most important health challenges in the world [6] and is the leading cause of death from single infectious agent [7]. The prevalence of TB differs in different parts of world. It has been reported that 22 countries in Eastern Mediterranean as well as Pakistan, Afghanistan, Egypt, Iraq, Iran, Morocco, Somalia, Sudan, and Yemen accounted for 95% of TB cases [11, 10, 9 ,8]. According to available statistics in Iran, Sistan and Baluchestan (n=330, 16.94 per 100000 people) and Golestan (n=428, 22.88 per 100000 people) provinces have the highest TB cases [12]. Golestan Province is a TB-endemic area of Iran with the highest TB prevalence [13]. Clinical symptoms of TB are often non-specific and include fever, night sweats, weight loss, anorexia, and fatigue [14]. Various factors such as age, thoracic radiological signs, the presence of a high number of bacilli in sputum smear of patients at the beginning of treatment, diabetes, immunosuppressive drugs, irregularities in the implementation of the treatment plan, or absence from treatment session affect the success or failure of TB treatment [13, 14, 15, 16, 17, 18, 19, 20, 21].
There are differences between diabetic patients and general population in the manifestation of symptoms of various comorbidities, including TB, such as lower prevalence, cough, sputum, and weight loss [22]. Among the cities of Golestan Province, Kordkuy has the highest prevalence of diabetes (8.1%) and refractory TB cases have been observed among diabetic patients in this city. The present study aims to screen pulmonary TB and determine the prevalence of TB in people with diabetes living in rural areas of Kordkuy City.
2. Materials and Methods This is a descriptive cross-sectional study, which was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1397.219). The study population included all diabetic patients living in 19 villages of Kordkuy city. Samples were selected using a census method. The exclusion criterion was pregnancy due to not being possible to do x-ray to prevent harm to the fetus. Informed consent was obtained from all participants. Data collection was carried out using a checklist, laboratory observations, chest x-ray (except for those forbidden to radiation exposure), TB skin test, and finally collecting sputum samples from patients who were more likely to be exposed to TB. The studied variables were: Age, gender, ethnicity, smoking, use of narcotic drugs or psychotropic substances, type of diabetes, duration of diabetes, history of previous TB, history and duration of contact with TB patients, sputum smear result, lung x-ray, last fasting blood sugar level, and last HbA1C test results. The collected data were analyzed in SPSS V. 16 software.
3. Results
Results showed that 77.4% of participants (n=716) were female, 98.2% (n=923) were Iranian nationals, and 886 (95.8%) were Persian. Demographic characteristics of participants are shown in Table 1.
Their mean age was 58.40 ±11.10 years with a mean diabetes duration of 8.5±39.47 years. Eight patients (0.9%) had kidney failure, none had acquired immunodeficiency disease, and 10 (1.1%) had a history of TB. We identified one case of active TB with smear-positive sputum. The patient was a 55-year-old woman, housekeeper, with Persian ethnicity, one year history of diabetes, and no history of contact with TB patients (Table 2).
4. Discussion and Conclusion
Recent studies have reported the prevalence of pulmonary TB in diabetic people is 4-5 times more than that in normal people [4]. Diabetes is a risk factor with indirect role in the development of TB [17]. In a study, the incidence of TB in diabetic group was 4.7 times higher than in non-diabetic people [21]. The current study revealed the relationship between diabetes and TB and showed that the TB prevalence was about 0.001 among diabetic patients. To better compare the prevalence of the disease in the same rural population and at the same time, pulmonary TB patients living in the village but had no diabetes were also examined. Study on some diabetic patients showed that there were confounding factors that made it more difficult to diagnose the disease. For example, addiction of the TB patient and his/her spouse led to the absence of some symptoms of TB in them. There have been contradictory results about the role of TB in the development of diabetes [17, 24]. Basoglu showed no significant difference between the two groups [22].
TB prevalence among diabetic people in Kordkuy city is 60 times higher. Both TB and diabetes are health risk factors. It is also recommended to conduct large-scale clinical studies in Iran to investigate other risk factors and TB symptoms in diabetic patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Ethics Code: IR.GUMSREC.1397.219).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all the officials of the centers, the volunteers, and all those who participated in the study and the efforts of Ms. Zeinab Khalilnejad.
References
- Kaynak I, Polat Ü. [Diabetes mellitus' lu hastaların tamamlayıcı ve alternatif tedavileri kullanma durumları ve diyabet tutumları ile ilişkisi (Turkish)]. Genel Tıp Dergisi. 2017; 27(2):56-64.[DOI:10.15321/GenelTipDer.2017.143]
- Critchley JA, Restrepo BI, Ronacher K, Kapur A, Bremer AA, Schlesinger LS, et al. Defining a research agenda to address the converging epidemics of tuberculosis and diabetes: part 1: epidemiology and clinical management. Chest. 2017; 152(1):165-73. [DOI:10.1016/j.chest.2017.04.155] [PMID] [PMCID]
- Kant S, Lata H, Natu SM, Mishra AK, Verma NS. Diabetes mellitus with pulmonary tuberculosis--a double trouble. Journal of the Indian Medical Association. 2013; 111(3):187-91. https://europepmc.org/article/med/24592761
- Asefzadeh MI, Bijani B, Kalantari Z. [Determine the prevalence of tuberculose infection in Diabetic Patients in Qazvin (Persian)]. Journal of Guilan University of Medical Sciences. 2008; 17(67):38-47. http://journal.gums.ac.ir/article-1-292-en.html
- Alisjahbana B, Sahiratmadja E, Nelwan EJ, Purwa AM, Ahmad Y, Ottenhoff TH, et al. The effect of type 2 diabetes mellitus on the presentation and treatment response of pulmonary tuberculosis. Clinical Infectious Diseases. 2007; 45(4):428-35. [DOI:10.1086/519841] [PMID]
- dos Santos MA, Albuquerque MF, Ximenes RA, Lucena-Silva NL, Braga C, Campelo AR, et al. Risk factors for treatment delay in pulmonary tuberculosis in Recife, Brazil. BMC Public Health. 2005; 5:25. [DOI:10.1186/1471-2458-5-25] [PMID] [PMCID]
- Morsy AM, Zaher HH, Hassan MH, Shouman A. Predictors of treatment failure among tuberculosis patients under DOTS strategy in Egypt. Eastern Mediterranean Health Journal. 2003; 9(4):689-701. [PMID]
- Vega Torres RA, Conde JG, Diaz M. Prevalence of tuberculin reactivity and risk factors for the development of active tuberculosis upon admission to a nursing home. Puerto Rico Health Sciences Journal. 1996; 15(4):275-7. [PMID]
- Chin C, Lee SS, Chen YS, Wann SR, Lin HH, Lin WR, et al. Mycobacteriosis in patients with fever of unknown origin. Journal of Microbiology, Immunology and Infection. 2003; 36(4):248-53. https://europepmc.org/article/med/14723253
- Bacakoğlu F, Başoğlu ÖK, Çok G, Sayıner A, Ateş M. Pulmonary tuberculosis in patients with diabetes mellitus. Respiration. 2001; 68(6):595-600. [DOI:10.1159/000050578] [PMID]
- Parwati I, van Crevel R, van Soolingen D. Possible underlying mechanisms for successful emergence of the Mycobacterium tuberculosis Beijing genotype strains. The Lancet Infectious Diseases. 2010; 10(2):103-11. [DOI:10.1016/S1473-3099(09)70330-5]
- Nosratollahi M, Khalileyan A. [The Survey of treatment outcome in TB Patients: the role of drug resistance and compliance with treatment regime in mazandaran province (Persian)]. Journal Urmia University of Medical Sciences. 2003; 14(4):9-15. http://umj.umsu.ac.ir/article-1-169-fa.html
- Golsha R, Rezaie Shirazi R, Shafiie A, Dashti M, Roshandel G. [Prevalence of Co-morbidities in Patients with Pulmonary Tuberculosis at 5th of Azar Hospital of Golestan Province of Iran (2001-2005) (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2009; 52(1):29-36. http://eprints.mums.ac.ir/7687/
- Rastegari S, Hosseinnezhad F, Faramarzi A, Baradaran B. [Evaluation of the tuberculosis epidemiology in diabetic patients at clinical and health centers in mashhad (Persian)]. Medical Journal of Mashhad University of Medical Sciences. 2014; 57(1):422-8. http://eprints.mums.ac.ir/7122/
- Biranvand E, Abediankenari S, Khalilian A, Biranvand B. [Risk factors for tuberculosis infection: a brief report (Persian)]. Tehran University of Medical Journal. 2012; 70(5):330-3. https://www.sid.ir/en/journal/ViewPaper.aspx?id=346280
- Dye C, Scheele S, Pathania V, Raviglione MC. Global burden of tuberculosis: Estimated incidence, prevalence, and mortality by country. Jama. 1999; 282(7):677-86. [DOI:10.1001/jama.282.7.677] [PMID]
- Jawad F, Shem AS, Memon R, Ansari G. Glucose intolerance in pulmonary tuberculosis. Journal of Pakistan Medical Association. 1995; 45(9):237-8. https://www.jpma.org.pk/article-details/4604
- Kermansaravi F, Metanat M. [Prevalence of Smear positive Pulmonary Tuberculosis among diabetic patients in Zahedan, Iran (2010-2011) (Persian)]. Journal Mazandaran University of Medical Sciences. 2012; 22(87):97-103. http://jmums.mazums.ac.ir/browse.php?a_id=812&sid=1&slc_lang=fa
- mansoori SD, Jamaati H, Arami S, Zadsar M, Abasian L, Estegamati A, et al. [Comparative study of the number and subgroup of lymphocytes in patient with type 2 diabetes mellitus pulmonary tuberculosis and diabetic patient with tuberculosis (Persian)]. Tanaffos. 2002; 1(4):45-50. https://www.sid.ir/fa/journal/ViewPaper.aspx?ID=43039
- Metanat M, Sharifimoud B, Parsi M, Sanei ME. [Effect of cigarette smoking on sputum smear conversion time among adult new pulmonary tuberculosis patients: A study from Iran Southeast (Persian)]. Iranian Journal of Clinical Infectious Diseases. 2010; 5(1):14-7. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=184546
- Shen TC, Lin CL, Wei CC, Liao WC, Chen WC, Chen CH, et al. Increased risk of tuberculosis in patients with type 1 diabetes mellitus: results from a population-based cohort study in Taiwan. Medicine. 2014; 93(16):e96. [DOI:10.1097/MD.0000000000000096] [PMID] [PMCID]
- Basoglu OK, Bacakoglu F, Cok G, Saymer A, Ates M. The oral glucose tolerance test in patients with respiratory infections. Monaldi Archives for Chest Disease. 1999; 54(4):307-10. http://europepmc.org/article/med/10546470
- Ronacher K, Joosten SA, van Crevel R, Dockrell HM, Walzl G, Ottenhoff TH. Acquired immunodeficiencies and tuberculosis: Focus on HIV/AIDS and diabetes mellitus. Immunological Reviews. 2015; 264(1):121-37. [DOI:10.1111/imr.12257] [PMID]
- Oluboyo PO, Erasmus RT. The significance of glucose intolerance in pulmonary tuberculosis. Tubercle. 1990; 71(2):135-8. [DOI:10.1016/0041-3879(90)90010-6]
Review Paper: Research |
Subject:
Special
Received: 2020/08/2 | Accepted: 2020/10/26 | Published: 2021/01/1
Received: 2020/08/2 | Accepted: 2020/10/26 | Published: 2021/01/1
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









