Volume 32, Issue 3 (10-2023)
JGUMS 2023, 32(3): 184-193 |
Back to browse issues page
Research code: 2987
Ethics code: IR.GUMS.REC.1399.398
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ashraf A, Ebrahimiyan Jektaji R, Saeedinia M, Biazar G, Eslami Kenarsari H, Behjat M K. Incidence of Barotrauma Following Mechanical Ventilation in Patients With COVID-19 Admitted to the ICUs of Two Selected Hospitals in Rasht, Iran. JGUMS 2023; 32 (3) :184-193
URL: http://journal.gums.ac.ir/article-1-2405-en.html
URL: http://journal.gums.ac.ir/article-1-2405-en.html
Ali Ashraf1 

 , Ramin Ebrahimiyan Jektaji2
, Ramin Ebrahimiyan Jektaji2 

 , Mostafa Saeedinia3
, Mostafa Saeedinia3 

 , Gelareh Biazar *4
, Gelareh Biazar *4 

 , Habib Eslami Kenarsari5
, Habib Eslami Kenarsari5 

 , Mohmmad Kazem Behjat6
, Mohmmad Kazem Behjat6 



 , Ramin Ebrahimiyan Jektaji2
, Ramin Ebrahimiyan Jektaji2 

 , Mostafa Saeedinia3
, Mostafa Saeedinia3 

 , Gelareh Biazar *4
, Gelareh Biazar *4 

 , Habib Eslami Kenarsari5
, Habib Eslami Kenarsari5 

 , Mohmmad Kazem Behjat6
, Mohmmad Kazem Behjat6 

1- Department of Anesthesiology, Faculty of Medicine, Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of General Surgery, Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Anesthesiology, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Statistics, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
6- Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of General Surgery, Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Anesthesiology, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Statistics, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
6- Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 3979 kb]
(524 Downloads)
| Abstract (HTML) (1612 Views)
Full-Text: (1411 Views)
Introduction
The SARS-CoV-2 coronavirus tends to the cells located in the lower respiratory tract and by multiplying in these areas; it causes lesions [3]. Studies have mentioned that providing appropriate, effective and safe respiratory support has been one of the biggest challenges for physicians during COVID-19 pandemic [5]. For treatment, oxygen therapy will be started at the rate of 5 liters per minute with a face mask or 5 to 10 liters per minute with a mask with a reserve bag and it will continue until the arterial blood oxygen saturation percentage is higher than or equal to 90% in adults or higher than 92 to 95% in pregnant women. If hypoxemia continues, despite high concentration oxygen therapy, it is recommended to use mechanical ventilation. Patients will be subjected to invasive or non-invasive treatments based on clinical conditions [6].
In the treatment process of hospitalized COVID-19 patients, one of the side effects that threaten patients is lung damage, like pressure trauma (barotrauma). Pulmonary barotrauma is a side effect of positive pressure mechanical ventilation that occurs because of alveolar rupture and leads to the release and accumulation of air in various extra alveolar spaces. As a result, complications such as pneumothorax, pneumomediastinum, and subcutaneous or mediastinal emphysema will occur [7, 8]. Alveolar rupture occurs due to excessive tidal volume during ventilation [9]. Studies have shown that in intubated COVID-19 patients, the risk of barotrauma is higher, which is associated with an increased rate of mortality [10]. Some studies have also associated barotrauma caused by COVID-19 with prolonged hospital and ICU stays. Respiratory failure in COVID-19 patients appears as severe hypoxemia. In mechanically ventilated patients, ARDS is the main risk factor for barotrauma [13].
Most COVID-19 patients experience symptoms of mild upper respiratory tract infection. However, a small proportion of patients with severe pneumonia and sepsis, develop multisystem failure with potential progression to ARDS. The development of ARDS and its related complications, which include septic shock, thrombotic complications, acute kidney injury, liver enzyme disorders, cardiac injury, and barotrauma, is associated with poor clinical outcomes in COVID-19 patients [14]. The prevalence of pneumothorax among COVID-19 patients in the intensive care unit has been reported as 2%, and in more recent studies, they found that the complications of barotrauma caused by invasive mechanical ventilation in COVID-19 patients have increased to 15% [15].
During the COVID-19 epidemic since 2020, there has been a significant increase in the number of ICU consultations with barotrauma symptoms in mechanically ventilated patients [7]. There are a limited number of studies on the epidemiology and potential risk factors associated with the development of barotrauma in COVID-19 patients [14]. In fact, the risk factors, pathophysiology and clinical consequences of barotrauma in patients with COVID-19 are still not well understood [8]. Due to the resurgence of COVID-19 disease and increase in the number of hospitalizations, in this study, patients diagnosed with COVID-19 hospitalized in the intensive care unit of Rasht educational and therapeutic hospitals were examined for the occurrence of barotrauma.
Methods
This retrospective study was conducted on 140 confirmed COVID-19 patients aged >18 years admitted to the intensive care units of Razi and Poursina hospitals in Rasht city in 2020. Medical records of the patients were checked and the demographic data plus underlying diseases including respiratory, cardiac, and metabolic diseases such as diabetes and hypertension were extracted using a checklist. Symptoms such as respiratory and gastrointestinal problems, cough, and fever were surveyed as well as the history of cigarette or opium smoking or drug abuse. The methods of oxygen administration and mechanical ventilation such (invasive or noninvasive) were also recorded. Pulmonary complications such as pneumothorax or subcutaneous emphysema were also recorded by an anesthesia assistant and the barotrauma was diagnosed. Data analyses were performed in SPSS software, version 22 (IBM Corp., Armonk, NY, USA). P<0.05 was considered statistically significant.
Results
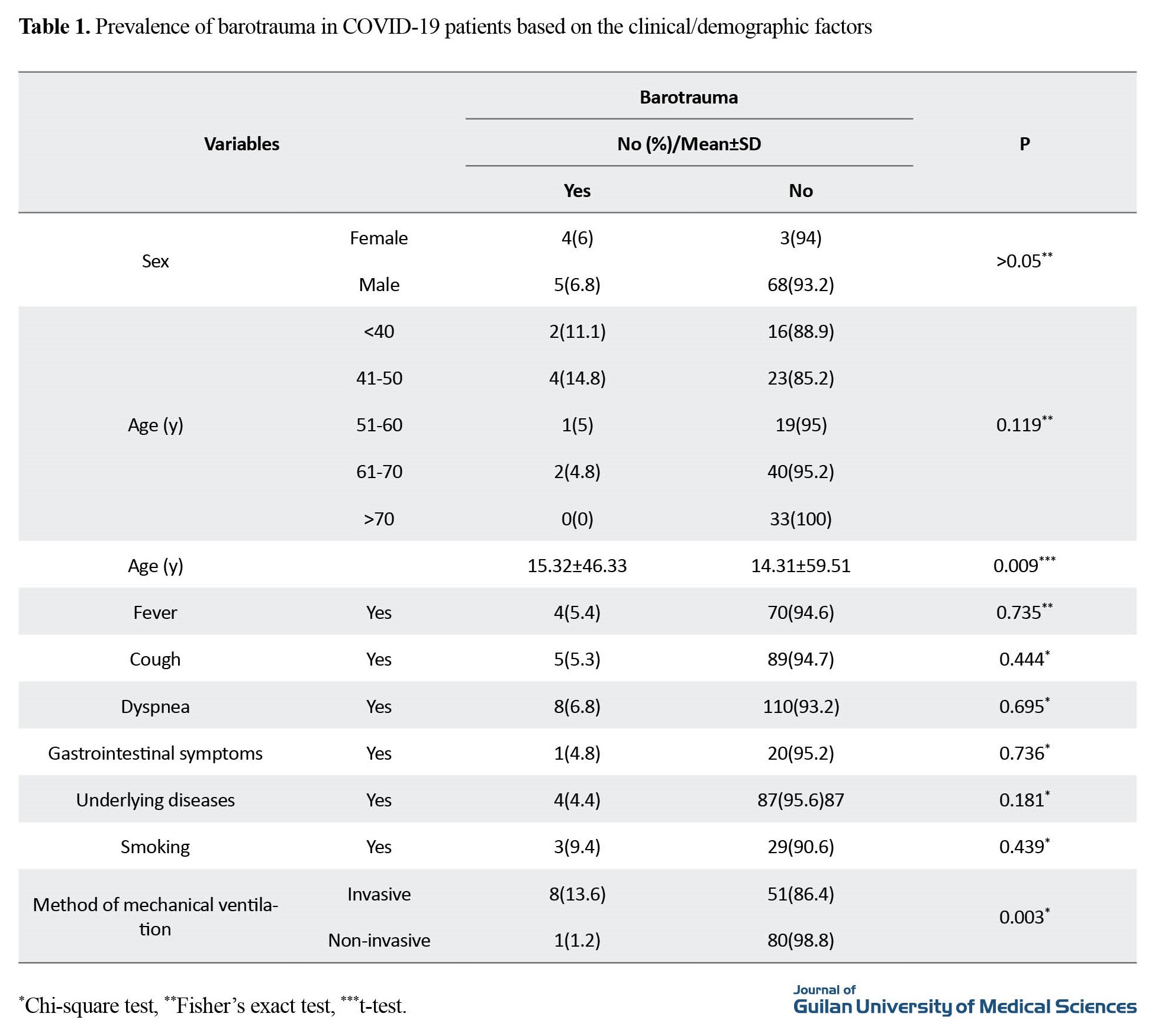
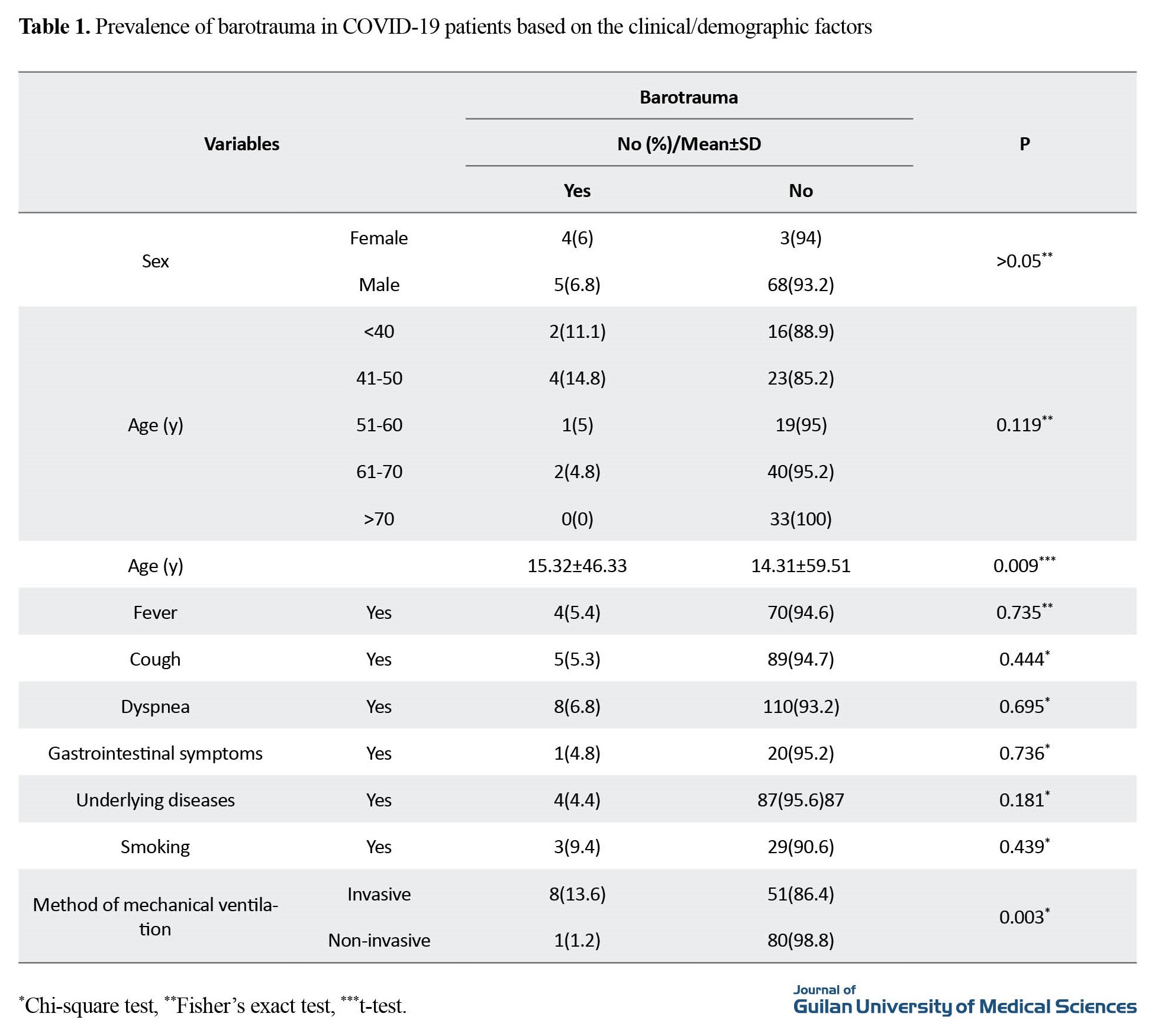
Out of 140 evaluated patients, 81 (57.9%) had non-invasive ventilation and 59(42.1%) had invasive ventilation. The barotrauma was reported in 9 cases (6.4%), 8(88.9%) in the form of pneumothorax and one (11.1%) had both pneumothorax and subcutaneous emphysema. The results showed that the incidence of barotrauma was significantly higher among patients who received invasive ventilation (P=0.003). No significant difference was observed in patients received non-invasive ventilation (P>0.05) (Table 1).
Conclusion
Following the selected treatments for hospitalized COVID-19 patients, a small percentage of them suffered pulmonary complications in the form of barotrauma, which can indicate proper performance and appropriate treatment decisions regarding changes in airway pressure. Despite the valuable information obtained from this study, some limitations can be considered. Due to the retrospective nature of the research, the consequences and associated factors were limited to the information that was recorded in the patients' files.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.398).
Funding
This study was funded by Guilan University of Medical Sciences.
Authors' contributions
Conceptualization, design, and supervision: Ali Ashraf and Gelareh Biazar; Methodology: Habib Eslami Kenarsari;Data collection, data analysis: Ramin Ebrahimiyan Jektaji and Mostafa Saeedinia; Drafting of the manuscript: Gelareh Biazar and Mohmmad Kazem Behjat; Editing & review: Mohmmad Kazem Behjat.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Clinical Research and Development Unit of Poursina Hospital and the Anesthesia Research Center of Guilan University of Medical Sciences, and the ICU staff of Poursina and Razi hospitals in Rasht for their cooperation in this study.
References
The SARS-CoV-2 coronavirus tends to the cells located in the lower respiratory tract and by multiplying in these areas; it causes lesions [3]. Studies have mentioned that providing appropriate, effective and safe respiratory support has been one of the biggest challenges for physicians during COVID-19 pandemic [5]. For treatment, oxygen therapy will be started at the rate of 5 liters per minute with a face mask or 5 to 10 liters per minute with a mask with a reserve bag and it will continue until the arterial blood oxygen saturation percentage is higher than or equal to 90% in adults or higher than 92 to 95% in pregnant women. If hypoxemia continues, despite high concentration oxygen therapy, it is recommended to use mechanical ventilation. Patients will be subjected to invasive or non-invasive treatments based on clinical conditions [6].
In the treatment process of hospitalized COVID-19 patients, one of the side effects that threaten patients is lung damage, like pressure trauma (barotrauma). Pulmonary barotrauma is a side effect of positive pressure mechanical ventilation that occurs because of alveolar rupture and leads to the release and accumulation of air in various extra alveolar spaces. As a result, complications such as pneumothorax, pneumomediastinum, and subcutaneous or mediastinal emphysema will occur [7, 8]. Alveolar rupture occurs due to excessive tidal volume during ventilation [9]. Studies have shown that in intubated COVID-19 patients, the risk of barotrauma is higher, which is associated with an increased rate of mortality [10]. Some studies have also associated barotrauma caused by COVID-19 with prolonged hospital and ICU stays. Respiratory failure in COVID-19 patients appears as severe hypoxemia. In mechanically ventilated patients, ARDS is the main risk factor for barotrauma [13].
Most COVID-19 patients experience symptoms of mild upper respiratory tract infection. However, a small proportion of patients with severe pneumonia and sepsis, develop multisystem failure with potential progression to ARDS. The development of ARDS and its related complications, which include septic shock, thrombotic complications, acute kidney injury, liver enzyme disorders, cardiac injury, and barotrauma, is associated with poor clinical outcomes in COVID-19 patients [14]. The prevalence of pneumothorax among COVID-19 patients in the intensive care unit has been reported as 2%, and in more recent studies, they found that the complications of barotrauma caused by invasive mechanical ventilation in COVID-19 patients have increased to 15% [15].
During the COVID-19 epidemic since 2020, there has been a significant increase in the number of ICU consultations with barotrauma symptoms in mechanically ventilated patients [7]. There are a limited number of studies on the epidemiology and potential risk factors associated with the development of barotrauma in COVID-19 patients [14]. In fact, the risk factors, pathophysiology and clinical consequences of barotrauma in patients with COVID-19 are still not well understood [8]. Due to the resurgence of COVID-19 disease and increase in the number of hospitalizations, in this study, patients diagnosed with COVID-19 hospitalized in the intensive care unit of Rasht educational and therapeutic hospitals were examined for the occurrence of barotrauma.
Methods
This retrospective study was conducted on 140 confirmed COVID-19 patients aged >18 years admitted to the intensive care units of Razi and Poursina hospitals in Rasht city in 2020. Medical records of the patients were checked and the demographic data plus underlying diseases including respiratory, cardiac, and metabolic diseases such as diabetes and hypertension were extracted using a checklist. Symptoms such as respiratory and gastrointestinal problems, cough, and fever were surveyed as well as the history of cigarette or opium smoking or drug abuse. The methods of oxygen administration and mechanical ventilation such (invasive or noninvasive) were also recorded. Pulmonary complications such as pneumothorax or subcutaneous emphysema were also recorded by an anesthesia assistant and the barotrauma was diagnosed. Data analyses were performed in SPSS software, version 22 (IBM Corp., Armonk, NY, USA). P<0.05 was considered statistically significant.
Results
Out of 140 evaluated patients, 81 (57.9%) had non-invasive ventilation and 59(42.1%) had invasive ventilation. The barotrauma was reported in 9 cases (6.4%), 8(88.9%) in the form of pneumothorax and one (11.1%) had both pneumothorax and subcutaneous emphysema. The results showed that the incidence of barotrauma was significantly higher among patients who received invasive ventilation (P=0.003). No significant difference was observed in patients received non-invasive ventilation (P>0.05) (Table 1).
Conclusion
Following the selected treatments for hospitalized COVID-19 patients, a small percentage of them suffered pulmonary complications in the form of barotrauma, which can indicate proper performance and appropriate treatment decisions regarding changes in airway pressure. Despite the valuable information obtained from this study, some limitations can be considered. Due to the retrospective nature of the research, the consequences and associated factors were limited to the information that was recorded in the patients' files.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.398).
Funding
This study was funded by Guilan University of Medical Sciences.
Authors' contributions
Conceptualization, design, and supervision: Ali Ashraf and Gelareh Biazar; Methodology: Habib Eslami Kenarsari;Data collection, data analysis: Ramin Ebrahimiyan Jektaji and Mostafa Saeedinia; Drafting of the manuscript: Gelareh Biazar and Mohmmad Kazem Behjat; Editing & review: Mohmmad Kazem Behjat.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Clinical Research and Development Unit of Poursina Hospital and the Anesthesia Research Center of Guilan University of Medical Sciences, and the ICU staff of Poursina and Razi hospitals in Rasht for their cooperation in this study.
References
- Kahn N. New virus discovered by Chinese scientists investigating pneumonia outbreak. 2020 [Updated 2020 January 8]. Available from: [Link]
- Gralinski LE, Menachery VD. Return of the coronavirus: 2019-nCoV. Viruses. 2020; 12(2):135. [DOI:10.3390/v12020135] [PMID] [PMCID]
- Mulangu S, Dodd LE, Davey RT Jr, Tshiani Mbaya O, Proschan M, Mukadi D, et al. A randomized, controlled trial of ebola virus disease therapeutics. The New England Journal of Medicine. 2019; 381(24):2293-303. [DOI:10.1056/NEJMoa1910993] [PMID]
- Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Bioscience Trends. 2020; 14(1):72-3. [DOI:10.5582/bst.2020.01047] [PMID]
- Volpicelli G, Lamorte A, Villén T. What's new in lung ultrasound during the COVID-19 pandemic. Intensive Care Medicine. 2020; 46(7):1445-8. [DOI:10.1007/s00134-020-06048-9] [PMID] [PMCID]
- World Health Organization. COVID-19 - China. 2020 [Updated 2020 January 12]. Available from: [Link]
- Edwards JA, Breitman I, Bienstock J, Badami A, Kovatch I, Dresner L, et al. Pulmonary barotrauma in mechanically ventilated coronavirus disease 2019 patients: A case series. Annals of Medicine and Surgery. 2020; 61:24-29. [DOI:10.1016/j.amsu.2020.11.054] [PMID] [PMCID]
- Shrestha DB, Sedhai YR, Budhathoki P, Adhikari A, Pokharel N, Dhakal R, et al. Pulmonary barotrauma in COVID-19: A systematic review and meta-analysis. Annals of Medicine and Surgery. 2022; 73:103221. [DOI:10.1016/j.amsu.2021.103221] [PMID] [PMCID]
- Wang XH, Duan J, Han X, Liu X, Zhou J, Wang X, et al. High incidence and mortality of pneumothorax in critically Ill patients with COVID-19. Heart & Lung. 2021; 50(1):37-43. [DOI:10.1016/j.hrtlng.2020.10.002] [PMID] [PMCID]
- Alhakeem A, Khan MM, Al Soub H, Yousaf Z. Case report: COVID-19-associated bilateral spontaneous pneumothorax-a literature review. The American Journal of Tropical Medicine and Hygiene. 2020; 103(3):1162-5. [DOI:10.4269/ajtmh.20-0680] [PMID] [PMCID]
- Carerj ML, Bucolo GM, Mazziotti S, Blandino A, Booz C, Cicero G, et al. Pulmonary barotrauma in patient suffering from COVID-19. Heliyon. 2022; 8(1):e08745. [DOI:10.1016/j.heliyon.2022.e08745] [PMID] [PMCID]
- McGuinness G, Zhan C, Rosenberg N, Azour L, Wickstrom M, Mason DM, et al. Increased incidence of barotrauma in patients with COVID-19 on invasive mechanical ventilation. Radiology. 2020; 297(2):E252-62. [DOI:10.1148/radiol.2020202352] [PMID] [PMCID]
- Carron M, Freo U, BaHammam AS, Dellweg D, Guarracino F, Cosentini R, et al. Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. British Journal of Anaesthesia. 2013; 110(6):896-914. [DOI:10.1093/bja/aet070] [PMID]
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020; 395(10229):1054-62. [DOI:10.1016/S0140-6736(20)30566-3] [PMID] [PMCID]
- Elsaaran H, AlQinai S, AlTarrah D, Abdulrasoul M, Al-Youha S, Almazeedi S, et al. Prevalence and risk factors of barotrauma in COVID-19 patients admitted to an intensive care unit in Kuwait; a retrospective cohort study. Annals of Medicine and Surgery. 2021; 63:102141. [DOI:10.1016/j.amsu.2021.01.089] [PMID] [PMCID]
- Wali A, Rizzo V, Bille A, Routledge T, Chambers AJ. Pneumomediastinum following intubation in COVID-19 patients: A case series. Anaesthesia. 2020; 75(8):1076-81. [DOI:10.1111/anae.15113] [PMID] [PMCID]
- Lyons C, Callaghan M. The use of high-flow nasal oxygen in COVID-19. Anaesthesia. 2020; 75(7):843-7. [DOI:10.1111/anae.15073] [PMID]
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020; 395(10223):507-13. [DOI:10.1016/S0140-6736(20)30211-7] [PMID]
- Udi J, Lang CN, Zotzmann V, Krueger K, Fluegler A, Bamberg F, et al. Incidence of barotrauma in patients with COVID-19 pneumonia during prolonged invasive mechanical ventilation - a case-control study. Journal of Intensive Care Medicine. 2021; 36(4):477-83. [DOI:10.1177/0885066620954364] [PMID]
- Anzueto A, Frutos-Vivar F, Esteban A, Alía I, Brochard L, Stewart T, et al. Incidence, risk factors and outcome of barotrauma in mechanically ventilated patients. Intensive Care Medicine. 2004; 30(4):612-9. [DOI:10.1007/s00134-004-2187-7] [PMID]
- Weg JG, Anzueto A, Balk RA, Wiedemann HP, Pattishall EN, Schork MA, et al. The relation of pneumothorax and other air leaks to mortality in the acute respiratory distress syndrome. The New England Journal of Medicine. 1998; 338(6):341-6. [DOI:10.1056/NEJM199802053380601] [PMID]
- Eisner MD, Thompson BT, Schoenfeld D, Anzueto A, Matthay MA; Acute Respiratory Distress Syndrome Network. Airway pressures and early barotrauma in patients with acute lung injury and acute respiratory distress syndrome. American Journal of Respiratory and Critical Care Medicine. 200; 165(7):978-82. [DOI:10.1164/ajrccm.165.7.2109059] [PMID]
- Niehaus M, Rusgo A, Roth K, Jacoby JL. Retropharyngeal air and pneumomediastinum: A rare complication of influenza A and asthma in an adult. The American Journal of Emergency Medicined. 2016; 34(2):338.e1-2. [DOI:10.1016/j.ajem.2015.06.020] [PMID]
- Sami R, Sereshti N. Case report: Barotrauma in COVID-19 case series. American Journal of Tropical Medicine and Hygiene. 2021; 105(1):54-58. [DOI:10.4269/ajtmh.21-0080] [PMID] [PMCID]
Review Paper: Research |
Subject:
Special
Received: 2021/09/14 | Accepted: 2023/02/5 | Published: 2023/10/1
Received: 2021/09/14 | Accepted: 2023/02/5 | Published: 2023/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |