Volume 31, Issue 1 (4-2022)
JGUMS 2022, 31(1): 2-17 |
Back to browse issues page
Research code: IR.SHMU.REC.1398.005
Ethics code: IR.SHMU.REC.1398.005
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Majidnia M, Kalteh Ei A, Nooreddini A, Kohi H. Prevalence of Maternal Anemia Among Pregnant Women in Golestan Province of Iran in 2020. JGUMS 2022; 31 (1) :2-17
URL: http://journal.gums.ac.ir/article-1-2449-en.html
URL: http://journal.gums.ac.ir/article-1-2449-en.html
1- Department of Epidemiology, School of Public Health, Shahroud University of Medical Sciences, Shahroud, Iran. , moustafa.majidnia@gmail.com
2- Department of Obstetrics and Gynecology, School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran.
3- Department of Nursing, School of Nursing and Midwifery, Hamedan University of Medical Science, Hamedan, Iran.
4- Azadshahr Health Center, School of Health, Golestan University of Medical Sciences, Gorgan, Iran.
2- Department of Obstetrics and Gynecology, School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran.
3- Department of Nursing, School of Nursing and Midwifery, Hamedan University of Medical Science, Hamedan, Iran.
4- Azadshahr Health Center, School of Health, Golestan University of Medical Sciences, Gorgan, Iran.
Full-Text [PDF 4899 kb]
(541 Downloads)
| Abstract (HTML) (1173 Views)
Full-Text: (753 Views)
Introduction
Nowadays, anemia is one of the most prevalent and important nutritional disorders in the world. Common causes of anemia are iron deficiency, infectious diseases, lack of essential nutrients (e.g. folate, vitamins A, B12, B6, C, E and D), blood diseases and acute/chronic infections [1 ,2 ,3]. Iron deficiency is the most common cause of anemia which is a serious public health problem mostly affecting children and pregnant women. World Health Organization estimates that 42% of children under the age of 5 years and 40% of pregnant women have anemia [5 ،4]. Considering the importance of anemia in pregnant women and since scant studies have been conducted on it in Golestan province of Iran, this study aims to assess the prevalence of maternal anemia and its related factors in pregnant women in Golestan province.
Methods
This cross-sectional analytical study was conducted on pregnant women referred to health centers affiliated to Golestan University of Medical Sciences whose information was registered in the Nab system and had medical records. Using the Environmental Performance Index (EPI) info software, a sample size of 821 was determined. To increase the validity of the study, the sample size increased to 1000. Information extracted from the medical records of pregnant women included: Location, age, interpregnancy interval, parity, education, place for receiving medical care, number of received medical care, history of urinary tract infection (UTI) before pregnancy, age of first pregnancy, age of marriage, and blood test results based on hematocrit, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration and red blood cell count. Chi-square test and multiple logistic regression analysis were used to find demographic/obstetric factors related to anemia.
Results
The results showed that the prevalence of anemia was 18.4%.; 19.27% had severe anemia, 63.03% had moderate anemia, and 17.7% had mild anemia. The mean age of pregnant women was 25±12.64 years. The interpregnancy interval, parity, age of first pregnancy, age of marriage, month of pregnancy, history of UTI before pregnancy, number of received medical care and education had statistically significant relationship with anemia in pregnant women according to the results of chi-square test (P<0.05). However, the place for receiving medical care and the place of residence had no statistically significant relationship with maternal anemia (P>0.05) (Table 1).
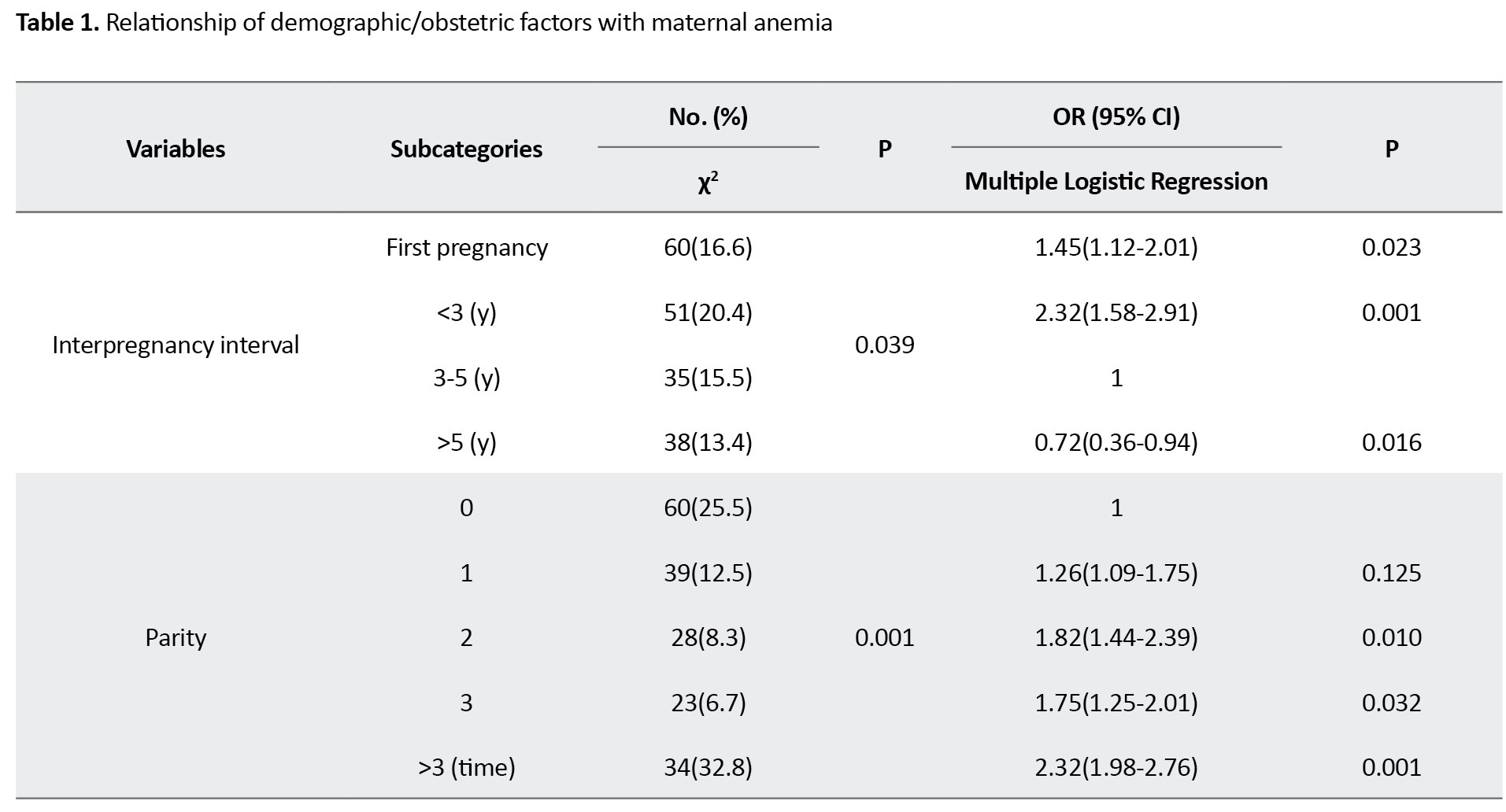
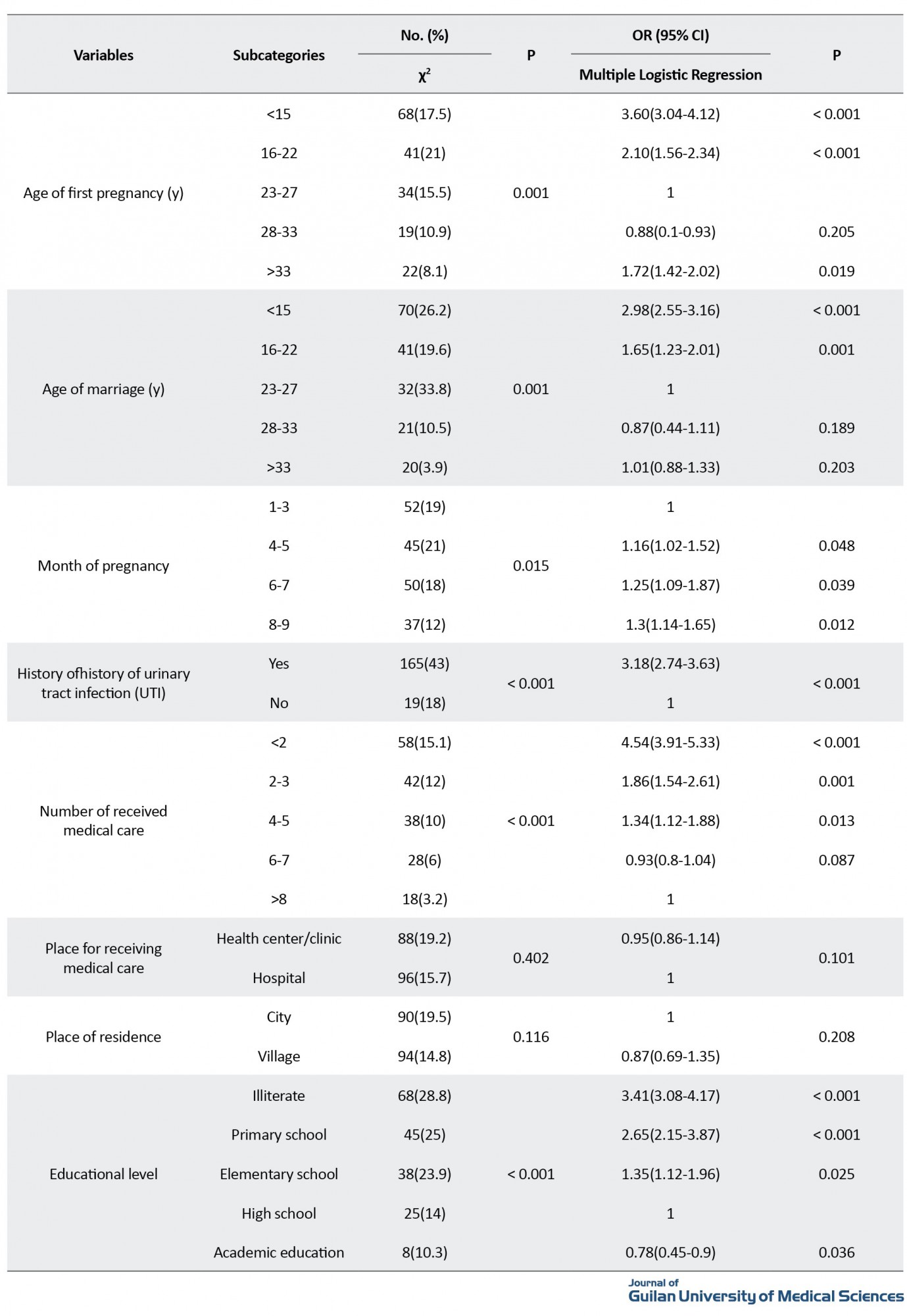
According to the multiple logistic regression analysis results, having a history of UTI before pregnancy increased the risk of maternal anemia by 3.18 times (95% CI=2.74-6.63). Regarding the number of received medical care, the number <2 increased the risk of maternal anemia by 4.54 times (95% CI=3.91-5.33). Education was also a strong predictor of anemia, such that pregnant women with academic education were 20% less likely to had anemia than those with high school education.
Discussion
The results of the present study showed a maternal anemia prevalence of 18.4%. The prevalence was significantly related to the interpregnancy interval, parity, age of first pregnancy, age of marriage, month of pregnancy, history of UTI before pregnancy, number of received medical care and education, but the place for receiving medical care and the place of residence had no statistically significant relationship with maternal anemia.
In a study by Vakili et al., the prevalence of anemia in Yazd province was reported 7.2%. In their study, the prevalence of anemia had no significant association with age, level of education, and occupation of the pregnant women, but varied significantly in urban areas [6]. This is against our results. The prevalence of anemia in the study by Latifi et al. in Bandar-e Turkmen was 13.4%, which is close to the rate reported in the present study. Consistent with the present study, they found that with increase in the pregnancy month, the prevalence of anemia increases due to the physiological needs, which requires the use of iron supplements [7]. There is a need for more interventional studies on maternal care and general health of pregnant women using a larger sample size at epidemiological levels and assessing the various causes of maternal anemia.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahroud University of Medical Sciences (Code: IR.SHMU.REC.1398.005).
Funding
This study is the result of the research project of the first author of the article, Mostafa Majidnia, Department of Epidemiology, Faculty of Health, Shahroud University of Medical Sciences, Shahroud.
Authors' contributions
Study design: Aylar Kalteh Ei and Mostafa Majidnia; Data collection, data analysis and data interpretation: Mostafa Majidnia; Writing the initial draft: Hasan Kohi and Ahmad Nooreddini; Review and final approval: All authors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank the Vice-Chancellor for Research and Technology of Golestan University of Medical Sciences and all women who participated in the study.
References
Nowadays, anemia is one of the most prevalent and important nutritional disorders in the world. Common causes of anemia are iron deficiency, infectious diseases, lack of essential nutrients (e.g. folate, vitamins A, B12, B6, C, E and D), blood diseases and acute/chronic infections [1 ,2 ,3]. Iron deficiency is the most common cause of anemia which is a serious public health problem mostly affecting children and pregnant women. World Health Organization estimates that 42% of children under the age of 5 years and 40% of pregnant women have anemia [5 ،4]. Considering the importance of anemia in pregnant women and since scant studies have been conducted on it in Golestan province of Iran, this study aims to assess the prevalence of maternal anemia and its related factors in pregnant women in Golestan province.
Methods
This cross-sectional analytical study was conducted on pregnant women referred to health centers affiliated to Golestan University of Medical Sciences whose information was registered in the Nab system and had medical records. Using the Environmental Performance Index (EPI) info software, a sample size of 821 was determined. To increase the validity of the study, the sample size increased to 1000. Information extracted from the medical records of pregnant women included: Location, age, interpregnancy interval, parity, education, place for receiving medical care, number of received medical care, history of urinary tract infection (UTI) before pregnancy, age of first pregnancy, age of marriage, and blood test results based on hematocrit, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration and red blood cell count. Chi-square test and multiple logistic regression analysis were used to find demographic/obstetric factors related to anemia.
Results
The results showed that the prevalence of anemia was 18.4%.; 19.27% had severe anemia, 63.03% had moderate anemia, and 17.7% had mild anemia. The mean age of pregnant women was 25±12.64 years. The interpregnancy interval, parity, age of first pregnancy, age of marriage, month of pregnancy, history of UTI before pregnancy, number of received medical care and education had statistically significant relationship with anemia in pregnant women according to the results of chi-square test (P<0.05). However, the place for receiving medical care and the place of residence had no statistically significant relationship with maternal anemia (P>0.05) (Table 1).
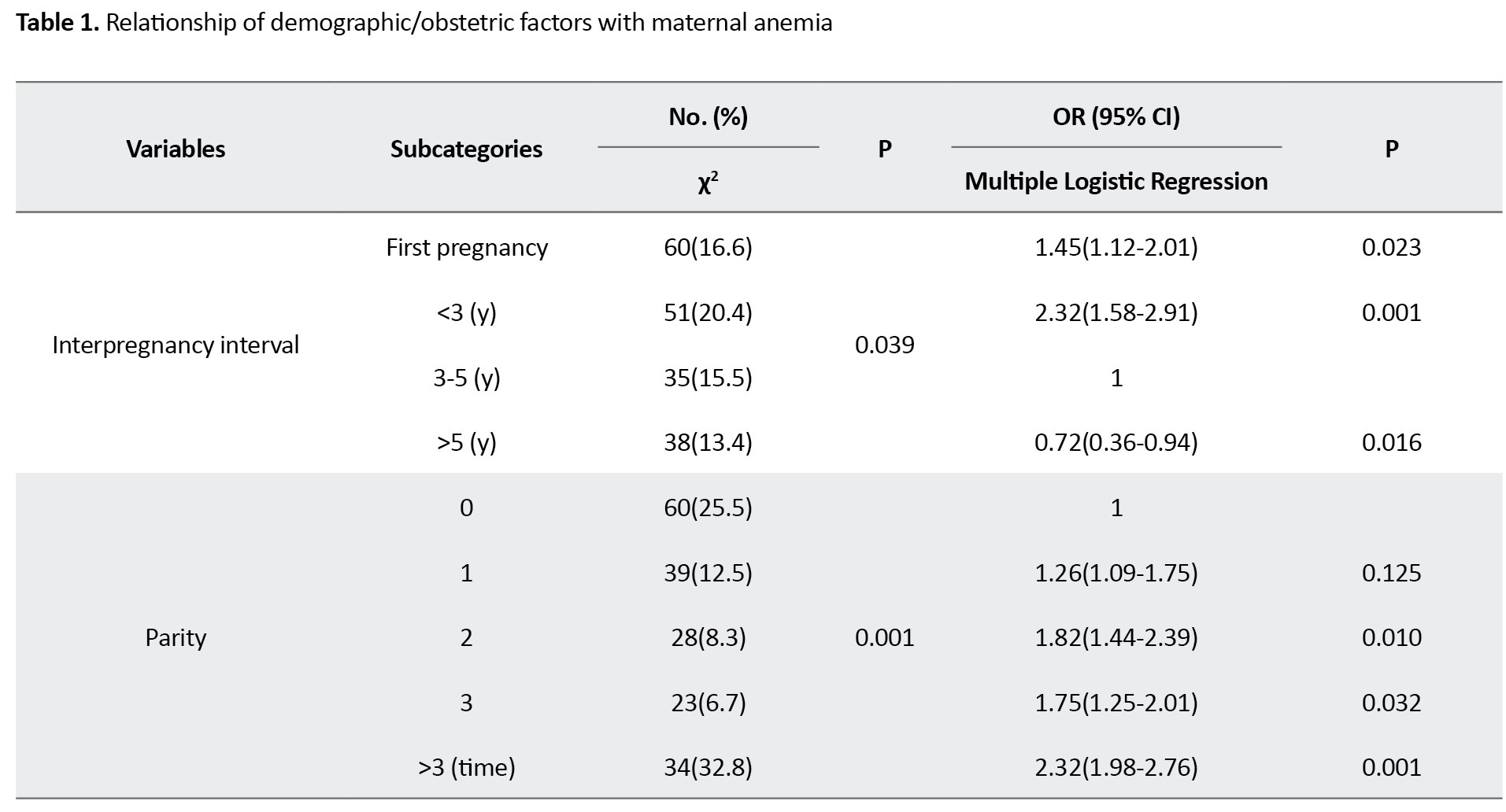
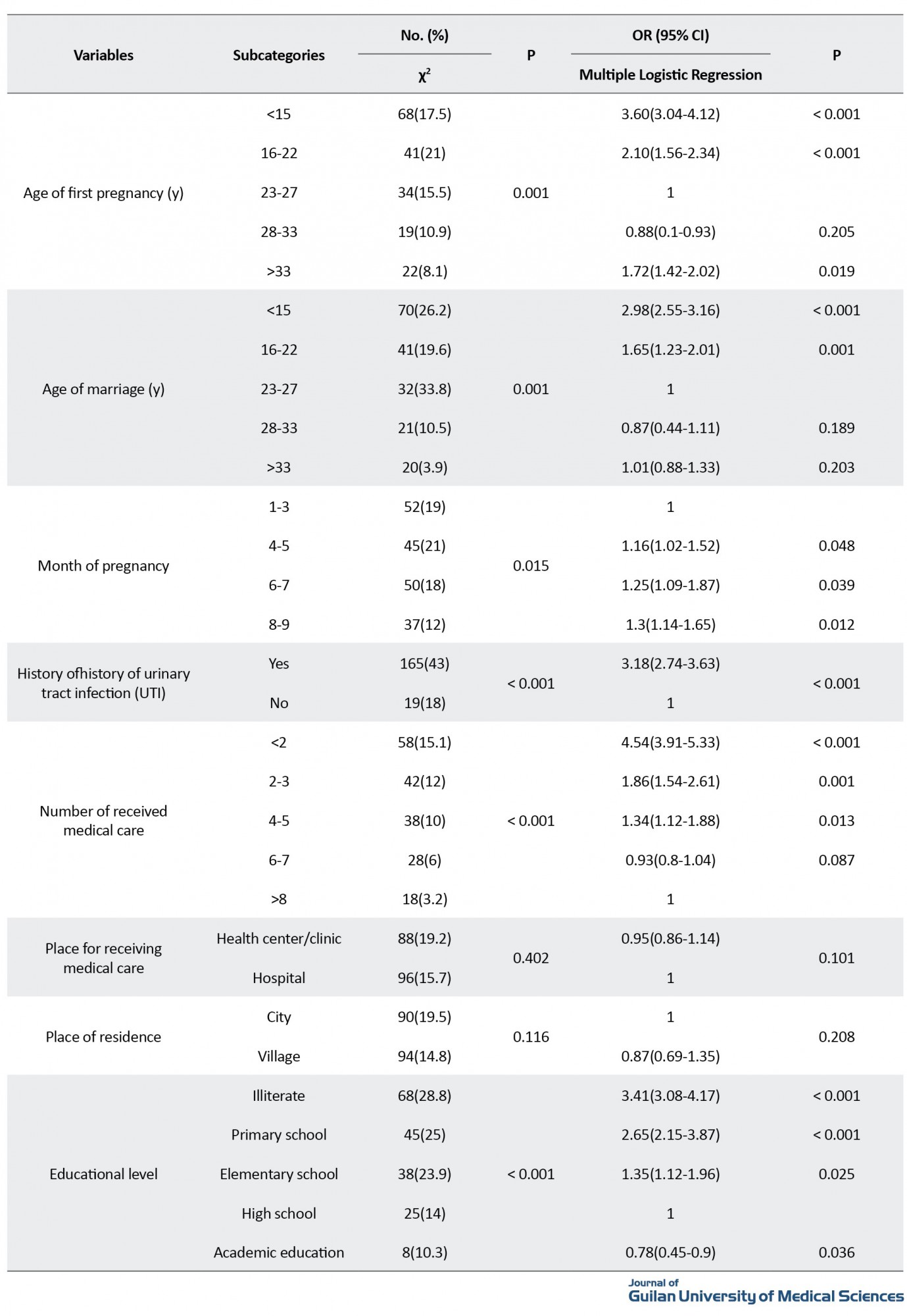
According to the multiple logistic regression analysis results, having a history of UTI before pregnancy increased the risk of maternal anemia by 3.18 times (95% CI=2.74-6.63). Regarding the number of received medical care, the number <2 increased the risk of maternal anemia by 4.54 times (95% CI=3.91-5.33). Education was also a strong predictor of anemia, such that pregnant women with academic education were 20% less likely to had anemia than those with high school education.
Discussion
The results of the present study showed a maternal anemia prevalence of 18.4%. The prevalence was significantly related to the interpregnancy interval, parity, age of first pregnancy, age of marriage, month of pregnancy, history of UTI before pregnancy, number of received medical care and education, but the place for receiving medical care and the place of residence had no statistically significant relationship with maternal anemia.
In a study by Vakili et al., the prevalence of anemia in Yazd province was reported 7.2%. In their study, the prevalence of anemia had no significant association with age, level of education, and occupation of the pregnant women, but varied significantly in urban areas [6]. This is against our results. The prevalence of anemia in the study by Latifi et al. in Bandar-e Turkmen was 13.4%, which is close to the rate reported in the present study. Consistent with the present study, they found that with increase in the pregnancy month, the prevalence of anemia increases due to the physiological needs, which requires the use of iron supplements [7]. There is a need for more interventional studies on maternal care and general health of pregnant women using a larger sample size at epidemiological levels and assessing the various causes of maternal anemia.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahroud University of Medical Sciences (Code: IR.SHMU.REC.1398.005).
Funding
This study is the result of the research project of the first author of the article, Mostafa Majidnia, Department of Epidemiology, Faculty of Health, Shahroud University of Medical Sciences, Shahroud.
Authors' contributions
Study design: Aylar Kalteh Ei and Mostafa Majidnia; Data collection, data analysis and data interpretation: Mostafa Majidnia; Writing the initial draft: Hasan Kohi and Ahmad Nooreddini; Review and final approval: All authors.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank the Vice-Chancellor for Research and Technology of Golestan University of Medical Sciences and all women who participated in the study.
References
- Mahmood T, Rehman AU, Tserenpil G, Siddiqui F, Ahmed M, Siraj F, et al. The association between iron-deficiency anemia and adverse pregnancy outcomes: A retrospective report from Pakistan. Cureus. 2019; 11(10):e5854. [DOI:10.7759/cureus.5854]
- World Health Organization. Assessing the iron status of populations: Including literature reviews. Geneva: World Health Organization; 2005. https://www.who.int/publications/i/item/9789241596107
- World Health Organization. Guideline: Daily iron supplementation in adult women and adolescent girls. Geneva: World Health Organization; 2016. https://apps.who.int/iris/handle/10665/204761
- Col Madendag I, Eraslan Sahin M, Madendag Y, Sahin E, Demir MB, Acmaz B, et al. The effect of iron deficiency anemia early in the third trimester on small for gestational age and birth weight: A retrospective cohort study on iron deficiency anemia and fetal weight. BioMed Research International. 2019; 2019:7613868. [PMID] [PMCID]
- UNICEF. Tracking progress on child and maternal nutrition: A survival and development priority. New York: UNICEF; 2009. https://data.unicef.org/resources/tracking-progress-child-maternal-nutrition-survival-development-priority/
- World Health Organization. Iron deficiency anemia: Assessment, prevention, and control. A guide for programme managers. Geneva: World Health Organization; 2001. https://apps.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/index.html
- Willard MD, Tvedten H. Small animal clinical diagnosis by laboratory methods. Amsterdam: Elsevier; 2012. https://www.google.com/books/edition/Small_Animal_Clinical_Diagnosis_by_Labor/o5PgygAACAAJ?hl=en
- Azami M, Darvishi Z, Sayehmiri K. Systematic review and meta-analysis of the prevalence of anemia among pregnant Iranian women (2005 - 2015). Shiraz E-Medical Journal. 2016; 17(4-5):e38462. [DOI:10.17795/semj38462]
- Berliner N, Benz EJ, Schiffman FJ. Anemia: Pathophysiology, diagnosis and management. Cambridge: Cambridge University Press; 2018. https://www.google.com/books/edition/Anemia/W1zOswEACAAJ?hl=en
- Breymann C. Iron deficiency and anaemia in pregnancy: Modern aspects of diagnosis and therapy. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2005; 123(SUPPLEMENT 2):S3-13. [DOI:10.1016/S0301-2115(05)80401-4]
- World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva: World Health Organization; 2011. https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf
- Bellos I, Pergialiotis V, Loutradis D, Papapanagiotou A, Daskalakis G. The role of hemoglobin degradation pathway in preeclampsia: A systematic review and meta-analysis. Placenta. 2020; 92:9-16. [DOI:10.1016/j.placenta.2020.01.014] [PMID]
- Randall DA, Patterson JA, Gallimore F, Morris JM, McGee TM, Ford JB, et al. The association between haemoglobin levels in the first 20 weeks of pregnancy and pregnancy outcomes. PloS One. 2019; 14(11):e0225123. [DOI:10.1371/journal.pone.0225123] [PMID] [PMCID]
- Parks S, Hoffman MK, Goudar SS, Patel A, Saleem S, Ali SA, et al. Maternal anaemia and maternal, fetal, and neonatal outcomes in a prospective cohort study in India and Pakistan. BJOG. 2019; 126(6):737-43. [DOI:10.1111/1471-0528.15585] [PMID] [PMCID]
- WHO. Anaemia. Geneva: WHO; 2020. https://www.who.int/health-topics/anaemia#tab=tab_1
- Abbasi A, Arooj S, Hussain W, Mughal AI, Habib N, Aziz W, et al . Causes of anemia in pregnant women of the state of azad kashmir: A cross-sectional survey. Health. 2013; 5(1):35-44. [DOI:10.4236/health.2013.51006]
- de Sá SA, Willner E, Duraes Pereira TA, de Souza VR, Teles Boaventura G, Blondet de Azeredo V. Anemia in pregnancy: Impact on weight and in the development of anemia in newborn. Nutrición Hospitalaria. 2015; 32(5):2071-9. [PMID]
- Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH. Anaemia in low-income and middle-income countries. The Lancet. 2011; 378(9809):2123-35. [DOI:10.1016/S0140-6736(10)62304-5]
- Geng F, Mai X, Zhan J, Xu L, Zhao Z, Georgieff M, et al. Impact of fetal-neonatal iron deficiency on recognition memory at 2 months of age. The Journal of Pediatrics. 2015; 167(6):1226-32. [DOI:10.1016/j.jpeds.2015.08.035] [PMID] [PMCID]
- Ren A, Wang J, Ye RW, Li S, Liu JM, Li Z. Low first-trimester hemoglobin and low birth weight, preterm birth and small for gestational age newborns. International Journal of Gynaecology and Obstetrics. 2007; 98(2):124-8. [DOI:10.1016/j.ijgo.2007.05.011] [PMID]
- Ali AA, Rayis DA, Abdallah TM, Elbashir MI, Adam I. Severe anaemia is associated with a higher risk for preeclampsia and poor perinatal outcomes in Kassala hospital, eastern Sudan. BMC Research Notes. 2011; 4:311. [DOI:10.1186/1756-0500-4-311] [PMID] [PMCID]
- Bora R, Sable C, Wolfson J, Boro K, Rao R. Prevalence of anemia in pregnant women and its effect on neonatal outcomes in Northeast India. The Journal of Maternal-Fetal & Neonatal Medicine. 2014; 27(9):887-91. [PMID]
- Nair M, Choudhury MK, Choudhury SS, Kakoty SD, Sarma UC, Webster P, et al. Association between maternal anaemia and pregnancy outcomes: A cohort study in Assam, India. BMJ Global Health. 2016; 1(1):e000026. [DOI:10.1136/bmjgh-2015-000026] [PMID] [PMCID]
- Pakniat H, Soofizadeh N, Movahed F. [Association of the first trimester anemia and fetal birth weight (Persian)]. Journal of Ilam University of Medical Sciences. 2018; 26(2):189-97. [DOI:10.29252/sjimu.26.2.189]
- Namazi A, Alizadeh S. [Health knowledge of pregnant women on anemia and its complication in pregnancy (Persian)]. Journal of Holistic Nursing and Midwifery. 2016; 26(2):98-106. http://hnmj.gums.ac.ir/article-1-692-en.html
- Sanayifar A, Emami Z, Rajabzade R, Sadeghi A, Hosseini SA. [The prevalence of anemia and some of its related factors in the pregnant women referred to Bojnurd Health and Treatment Centers, 2014 (Persian)]. Sadra Medical Sciences Journal. 2015; 3(4):235-46. https://smsj.sums.ac.ir/article_44069.html?lang=en
- Vakili M, Mardani Z, Mirzaei M. [Frequency of anemia in the pregnant women referring to the health centers in Yazd, Iran (2016-2017) (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2018; 21(2):9-15. [DOI:10.22038/IJOGI.2018.10701]
- Rajabzadeh R, Hoseini SH, Rezazadeh J, Baghban A, Nasiri M, Hosein Ayati M. [Prevalence of anemia and its related factors in pregnant women referring to health centers of Mane and Samalghan city (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2015;18(171):1-7. [DOI:10.22038/IJOGI.2015.6133]
- Mostajeran M, Hassanzadeh A, Toloei Azar A, Majlessi F, Shariat M, Aghdak P. [Prevalence of iron deficiency anemia in unwanted and high risk pregnancies in Isfahan Province, Iran (Persian)]. Health System Research. 2013; 9(1):66-75. https://www.sid.ir/En/Journal/ViewPaper.aspx?ID=333345
- Esmat B, Mohammad R, Behnam S, Shahrzad M, Soodabeh T, Minoo A, et al. Prevalence of iron deficiency anemia among Iranian pregnant women; a systematic review and meta-analysis. Journal of Reproduction & Infertility. 2010; 11(1):17-24. [PMID]
- Melku M, Addis Z, Alem M, Enawgaw B. Prevalence and predictors of maternal anemia during pregnancy in Gondar, Northwest Ethiopia: An institutional based cross-sectional study. Anemia. 2014; 2014:108593. [DOI:10.1155/2014/108593] [PMID] [PMCID]
- Lokare PO, Karanjekar VD, Gattani PL, Kulkarni AP. A study of prevalence of anemia and sociodemographic factors associated with anemia among pregnant women in Aurangabad city, India. Annals of Nigerian Medicine. 2012; 6(1):30-4. [DOI:10.4103/0331-3131.100213]
- Dim CC, Onah HE. The prevalence of anemia among pregnant women at booking in Enugu, South Eastern Nigeria. MedGenMed : Medscape General Medicine. 2007; 9(3):11. [PMID]
- Latifi M, Kamran Toraj M, Charkazi A, Graylou S. [Prevalence of iron deficiency anemia in pregnant women referred to health centers in Bandar Turkmen in 2013 (Persian)]. Jorjani Biomedicine Journal. 2016; 4(2):100-5. http://goums.ac.ir/jorjanijournal/article-1-479-en.html
- Saghafi N, Mihan S, Abrishami F. [Assessment of the prevalence of iron deficiency anemia in pregnant women referring to Ghaem Hospital (Persian)]. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2015; 18(163):1-7. [DOI:10.22038/IJOGI.2015.5332]
- Gorgani F, Majlessi F, Momeni MK, Tol A, Rahimi Foroshani A. [Prevalence of anemia and some related factor in pregnant woman referred to health centers affiliated to Zahedan University of Medical Sciences in 2013 (Persian)]. Razi Journal of Medical Sciences. 2016; 22(141):47-58. http://rjms.iums.ac.ir/article-1-3306-en.html
- Ayoya MA, Spiekermann-Brouwer GM, Traoré AK, Stoltzfus RJ, Garza C. Determinants of anemia among pregnant women in Mali. Food and Nutrition Bulletin. 2006; 27(1):3-11. [PMID]
- Yaghoobi H, Zolfizadeh F, Asadollahi Z, Vazirinejad R, Rezaeian M. Prevalence of iron deficiency anemia and some related factors among pregnant women referred to healthcare centers in Bandar Lengeh, Iran, in 2015. Journal of Occupational Health and Epidemiology. 2015; 4(2):92-100. [DOI:10.18869/acadpub.johe.4.2.92]
Review Paper: Research |
Subject:
Special
Received: 2021/12/18 | Accepted: 2022/02/23 | Published: 2022/04/1
Received: 2021/12/18 | Accepted: 2022/02/23 | Published: 2022/04/1
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









