Volume 32, Issue 2 (7-2023)
JGUMS 2023, 32(2): 140-151 |
Back to browse issues page
Research code: 188
Ethics code: IR.GUMS.REC.1398.025
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Asadi K, Fallah Khosh Ghalb M, Cyrus K. Comparison of the Clinical Outcomes of Plastering and Bandage Treatment Methods in Patients With Ankle Sprains: A Randomized Clinical Trial Study. JGUMS 2023; 32 (2) :140-151
URL: http://journal.gums.ac.ir/article-1-2483-en.html
URL: http://journal.gums.ac.ir/article-1-2483-en.html
1- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran., kasadi67@yahoo.com
2- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran., masoud.khoshghalb@yahoo.com
3- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran., masoud.khoshghalb@yahoo.com
3- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 4169 kb]
(495 Downloads)
| Abstract (HTML) (1805 Views)
Full-Text: (924 Views)
Introduction
Musculoskeletal injuries can lead to many disabilities affecting the individual, society, and healthcare systems. The ankle is one of the most common anatomical parts of the body that is injured in active people, such as people with sports and military activities [1, 2]. In the United States, 23,000 cases of ankle sprains occur daily [4]. Meanwhile, the treatment measures for ankle sprains are different based on the severity of the injury and the symptoms of the patients. Treatment measures for ankle sprains include care recommendations, symptomatic therapy, joint immobilization using bandages and plasters, and reconstructive surgery. On the other hand, failing to properly treat the patient can lead to the recurrence of the condition and, as a result, instability of the joint [9, 10]. The most common treatment solution in this condition is to immobilize the joint using a short plaster from the base of the toes to the tibia bone and a bandage from the middle of the foot to the ankle [11, 12]. Therefore, the present study was conducted to evaluate and compare the effects of two treatment methods bandage and plaster in patients with ankle injuries in terms of pain rate, duration of activity restriction, and ankle-hindfoot scale (AHS).
Methods
In a randomized controlled clinical trial study, two therapeutic methods of bandaging and plastering were investigated for the treatment of ankle sprains in 78 patients who were referred to the emergency department of Poursina Hospital in Rasht, Iran. The inclusion criteria included patients aged 20 to 50 years with complaints of 1- and 2-degree sprains, which occurred less than 48 hours after the sprain. Exclusion criteria included patients with neuropathy, varicose veins of the affected limb, diabetes, a history of ankle fracture, a history of previous sprain, and a history of previous surgery, patients requiring surgery, and sedentary patients. In this study, convenience sampling was used to select participants. The patients who met the inclusion criteria were divided into two groups of A (plaster) and B (bandage) by a simple random method, and 3, 6, and 12 weeks after the start of the treatment, they were examined for the level of pain. Finally, patients were evaluated in terms of pain level using the visual analogue scale (VAS), range of motion (based on the degree of plantar and dorsiflexion), tenderness level, and return to work. Data were analyzed using IBM SPSS software, version 20. The Kolmogorov-Smirnov test was used to check the normality of the data. Data were presented using frequency (percentage) and Mean±SD. Due to the non-normal distribution of the data, the Mann-Whitney test was used to compare the duration of activity restriction between the two groups. A chi-square test was used to compare the frequency of members in the two studied groups. Repeated-measures ANOVA was used to compare the mean of dependent variables (pain and AHS) in two treatment groups. The significance level was set at P<0.05 for all statistical tests.
Results
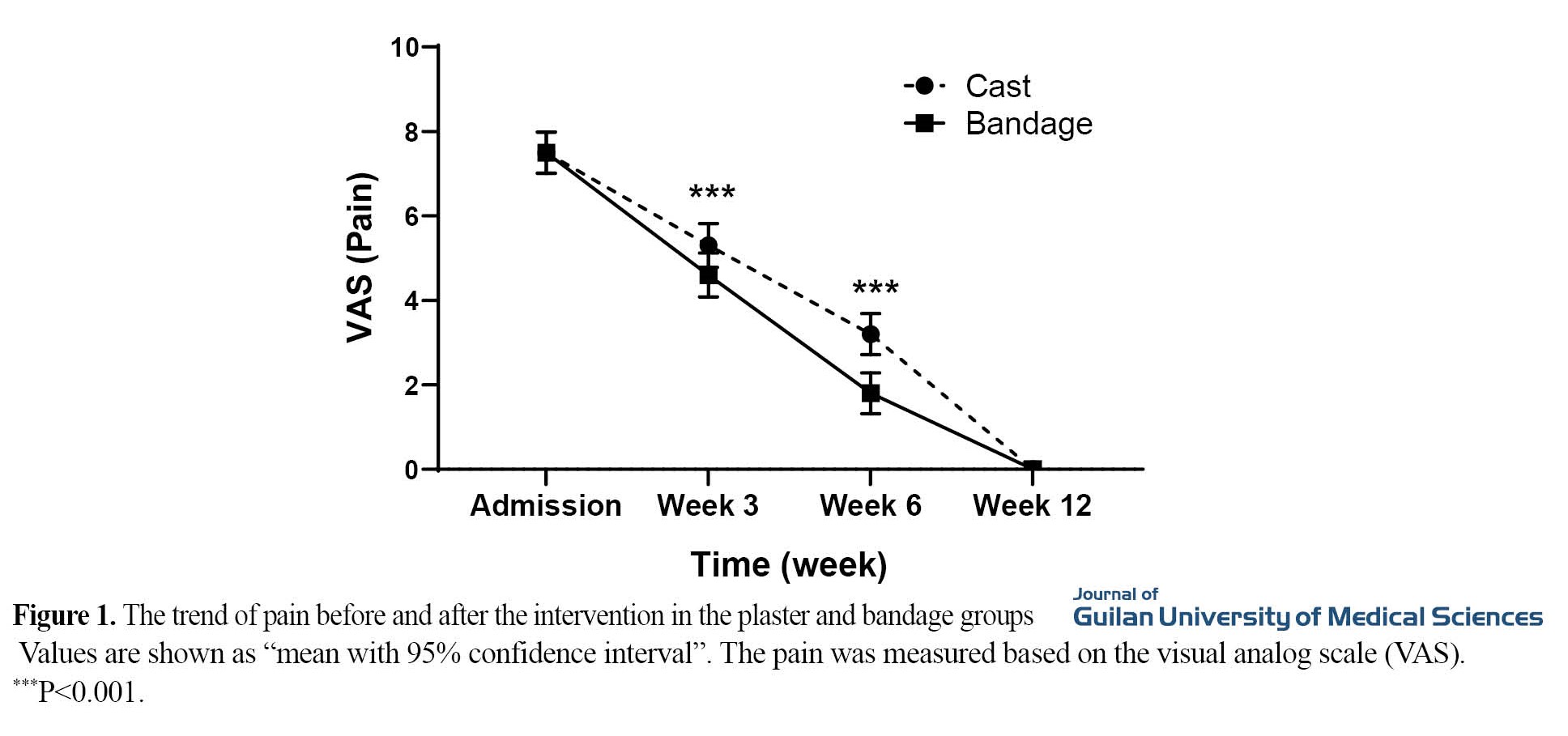
A total of 78 patients participated in the present study. Patients were divided into two treatment groups: Bandage (n=39) and plaster (n=39). Based on the repeated-measures ANOVA, the rate of pain had a decreasing trend in the two groups in both the bandage and plaster groups (P<0.001). In general, the rate of pain based on the VAS in the bandage was lower than the average in the plaster, and the trend of pain reduction in the bandage group had a steeper slope than in the plaster group. Also, the rate of pain at the time of admission was not significantly different between the two treatment groups (P=0.760). However, after three and six weeks of treatment, the pain level in the bandage group was significantly lower than in the plaster group (P<0.001). Twelve weeks after the treatment, there was no significant difference in the amount of pain in the two groups (P=0.999) (Figure 1). Based on the repeated-measures ANOVA results, the AHS score during 3-12 weeks had a significant increasing trend in the bandage and plaster groups. However, the group did not have a significant effect on the AHS level (P=0.32). In general, time had no significant effect on AHS scores (P=0.610) and study groups (P=0.072). In addition, the duration of activity restriction in the plaster group had a significantly lower mean than in the bandage group (P=0.002).
Discussion
Based on the findings of the present study, the rate of pain had a decreasing trend in both the bandage and plaster groups, which was statistically significant. In general, the rate of pain based on the VAS score in the bandage group was lower than the average score in the plaster group, and the trend of pain reduction in the bandage group had a steeper slope than in the plaster group. Also, after three and six weeks of treatment, the pain level in the bandage group was significantly lower than in the plaster group, which was statistically significant. This finding was consistent with the results of a study by Almedia et al. [20]. They showed that pain intensity based on VAS was lower in the bandage group than in the plaster group two weeks, one month, and three months after the start of treatment. Also, another study by Saltzman et al. [18] showed that the intensity of pain in the bandage group was lower than in the plaster group. The greater pain intensity of the plaster group can be due to its greater hardness.
Based on the findings of the present study, the AHS score from three weeks to 12 weeks had a significant increasing trend in the bandage and plaster groups. In addition, the duration of activity restriction in the plaster group had a significantly lower mean than in the bandage group. Verhagen et al. showed that the average duration of activity restriction in the plaster group was less than that of the bandage group [16]. This finding could be due to the shorter treatment period in the plaster group compared to the bandage group [16]. On the other hand, Kannus and Renstrom [4] showed that the length of recovery in the plaster group was shorter than in the bandage group. These differences can be due to differences in the type and degree of torsion in different studies [4].
In summary, plastering treatment reduces the days of activity limitation and patients return to work and daily activities faster. However, plastering has limitations, such as more cost and also, limiting the movements of the limbs, for a logical conclusion. There is a need for more studies considering all aspects of applying bandage and plastering methods in ankle sprain
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Guilan University of Medical Sciences (IR.GUMS.REC.1398.025) and registered at the Iranian Registry of Clinical Trials (Code: IRCT20190529043760N1).
Funding
The present research was funded by the Research and Technology Vice-Chancellor of Guilan University of Medical Sciences.
Authors' contributions
Study design, writing the initial draft, review and final approval: All authors; Data collection, data analysis, and data interpretation: Kamran Asadi and Khashayar Cyrus.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the officials of Guilan University of Medical Sciences and all the participants in this study.
References
Musculoskeletal injuries can lead to many disabilities affecting the individual, society, and healthcare systems. The ankle is one of the most common anatomical parts of the body that is injured in active people, such as people with sports and military activities [1, 2]. In the United States, 23,000 cases of ankle sprains occur daily [4]. Meanwhile, the treatment measures for ankle sprains are different based on the severity of the injury and the symptoms of the patients. Treatment measures for ankle sprains include care recommendations, symptomatic therapy, joint immobilization using bandages and plasters, and reconstructive surgery. On the other hand, failing to properly treat the patient can lead to the recurrence of the condition and, as a result, instability of the joint [9, 10]. The most common treatment solution in this condition is to immobilize the joint using a short plaster from the base of the toes to the tibia bone and a bandage from the middle of the foot to the ankle [11, 12]. Therefore, the present study was conducted to evaluate and compare the effects of two treatment methods bandage and plaster in patients with ankle injuries in terms of pain rate, duration of activity restriction, and ankle-hindfoot scale (AHS).
Methods
In a randomized controlled clinical trial study, two therapeutic methods of bandaging and plastering were investigated for the treatment of ankle sprains in 78 patients who were referred to the emergency department of Poursina Hospital in Rasht, Iran. The inclusion criteria included patients aged 20 to 50 years with complaints of 1- and 2-degree sprains, which occurred less than 48 hours after the sprain. Exclusion criteria included patients with neuropathy, varicose veins of the affected limb, diabetes, a history of ankle fracture, a history of previous sprain, and a history of previous surgery, patients requiring surgery, and sedentary patients. In this study, convenience sampling was used to select participants. The patients who met the inclusion criteria were divided into two groups of A (plaster) and B (bandage) by a simple random method, and 3, 6, and 12 weeks after the start of the treatment, they were examined for the level of pain. Finally, patients were evaluated in terms of pain level using the visual analogue scale (VAS), range of motion (based on the degree of plantar and dorsiflexion), tenderness level, and return to work. Data were analyzed using IBM SPSS software, version 20. The Kolmogorov-Smirnov test was used to check the normality of the data. Data were presented using frequency (percentage) and Mean±SD. Due to the non-normal distribution of the data, the Mann-Whitney test was used to compare the duration of activity restriction between the two groups. A chi-square test was used to compare the frequency of members in the two studied groups. Repeated-measures ANOVA was used to compare the mean of dependent variables (pain and AHS) in two treatment groups. The significance level was set at P<0.05 for all statistical tests.
Results
A total of 78 patients participated in the present study. Patients were divided into two treatment groups: Bandage (n=39) and plaster (n=39). Based on the repeated-measures ANOVA, the rate of pain had a decreasing trend in the two groups in both the bandage and plaster groups (P<0.001). In general, the rate of pain based on the VAS in the bandage was lower than the average in the plaster, and the trend of pain reduction in the bandage group had a steeper slope than in the plaster group. Also, the rate of pain at the time of admission was not significantly different between the two treatment groups (P=0.760). However, after three and six weeks of treatment, the pain level in the bandage group was significantly lower than in the plaster group (P<0.001). Twelve weeks after the treatment, there was no significant difference in the amount of pain in the two groups (P=0.999) (Figure 1). Based on the repeated-measures ANOVA results, the AHS score during 3-12 weeks had a significant increasing trend in the bandage and plaster groups. However, the group did not have a significant effect on the AHS level (P=0.32). In general, time had no significant effect on AHS scores (P=0.610) and study groups (P=0.072). In addition, the duration of activity restriction in the plaster group had a significantly lower mean than in the bandage group (P=0.002).
Discussion
Based on the findings of the present study, the rate of pain had a decreasing trend in both the bandage and plaster groups, which was statistically significant. In general, the rate of pain based on the VAS score in the bandage group was lower than the average score in the plaster group, and the trend of pain reduction in the bandage group had a steeper slope than in the plaster group. Also, after three and six weeks of treatment, the pain level in the bandage group was significantly lower than in the plaster group, which was statistically significant. This finding was consistent with the results of a study by Almedia et al. [20]. They showed that pain intensity based on VAS was lower in the bandage group than in the plaster group two weeks, one month, and three months after the start of treatment. Also, another study by Saltzman et al. [18] showed that the intensity of pain in the bandage group was lower than in the plaster group. The greater pain intensity of the plaster group can be due to its greater hardness.
Based on the findings of the present study, the AHS score from three weeks to 12 weeks had a significant increasing trend in the bandage and plaster groups. In addition, the duration of activity restriction in the plaster group had a significantly lower mean than in the bandage group. Verhagen et al. showed that the average duration of activity restriction in the plaster group was less than that of the bandage group [16]. This finding could be due to the shorter treatment period in the plaster group compared to the bandage group [16]. On the other hand, Kannus and Renstrom [4] showed that the length of recovery in the plaster group was shorter than in the bandage group. These differences can be due to differences in the type and degree of torsion in different studies [4].
In summary, plastering treatment reduces the days of activity limitation and patients return to work and daily activities faster. However, plastering has limitations, such as more cost and also, limiting the movements of the limbs, for a logical conclusion. There is a need for more studies considering all aspects of applying bandage and plastering methods in ankle sprain
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Guilan University of Medical Sciences (IR.GUMS.REC.1398.025) and registered at the Iranian Registry of Clinical Trials (Code: IRCT20190529043760N1).
Funding
The present research was funded by the Research and Technology Vice-Chancellor of Guilan University of Medical Sciences.
Authors' contributions
Study design, writing the initial draft, review and final approval: All authors; Data collection, data analysis, and data interpretation: Kamran Asadi and Khashayar Cyrus.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the officials of Guilan University of Medical Sciences and all the participants in this study.
References
- Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Medicine. 2007; 37(1):73-94. [Link]
- Lievers WB, Adamic PF. Incidence and severity of foot and ankle injuries in men's collegiate American football. Orthopaedic Journal of Sports Medicine. 2015; 3(5):2325967115581593. [DOI:10.1177/2325967115581593] [PMID] [PMCID]
- Nabian MH, Zadegan SA, Zanjani LO, Mehrpour SR. Epidemiology of joint dislocations and ligamentous/tendinous injuries among 2,700 patients: Five-Year trend of a tertiary center in Iran. Archives of Bone and Joint Surgery. 2017; 5(6):426-34. [PMCID]
- Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization.The Journal of Bone & Joint Surgery. 1991; 73(2):305-12. [DOI:10.2106/00004623-199173020-00021] [PMID]
- Garrick JG, Requa RK. The epidemiology of foot and ankle injuries in sports. Clinics in Sports Medicine. 1988; 7(1):29-36. [DOI:10.1016/S0278-5919(20)30956-X]
- Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. The American Journal of Sports Medicine. 1977; 5(6):241-2. [DOI:10.1177/036354657700500606] [PMID]
- Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bulletin of the NYU Hospital for Joint Diseases. 2011; 69(1):17-26. [Link]
- Hubbard-Turner T, Wikstrom EA, Guderian S, Turner MJ. An acute lateral ankle sprain significantly decreases physical activity across the lifespan. Journal of Sports Science & Medicine. 2015; 14(3):556-61. [PMCID]
- Petersen W, Rembitzki IV, Koppenburg AG, Ellermann A, Liebau C, Brüggemann GP, et al. Treatment of acute ankle ligament injuries: A systematic review. Archives of Orthopaedic and Trauma Surgery. 2013; 133(8):1129-41. [PMID] [PMCID]
- Barg A, Tochigi Y, Amendola A, Phisitkul P, Hintermann B, Saltzman CL. Subtalar instability: Diagnosis and treatment. Foot & Ankle International. 2012; 33(2):151-60. [DOI:10.3113/FAI.2012.0151] [PMID]
- Clanton TO. Athletic injuries to the soft tissues of the foot and ankle. Surgery of the Foot and Ankle. 1999; 1090-209. [Link]
- Clanton TO, Campbell KJ, Wilson KJ, Michalski MP, Goldsmith MT, Wijdicks CA, et al. Qualitative and quantitative anatomic investigation of the lateral ankle ligaments for surgical reconstruction procedures.The Journal of Bone and Joint Surgery. 2014; 96(12):e98. [DOI:10.2106/JBJS.M.00798] [PMID]
- Gay A, Culliford D, Leyland K, Arden NK, Bowen CJ. Associations Between body mass index and foot joint pain in middle-aged and older women: A longitudinal population-based cohort study. Arthritis Care & Research. 2014; 66(12):1873-9. [DOI:10.1002/acr.22408] [PMID] [PMCID]
- Hawke F, Rome K, Evans AM. The relationship between foot posture, body mass, age and ankle, lower-limb and whole-body flexibility in healthy children aged 7 to 15 years. Journal of Foot and Ankle Research. 2016; 9:14. [PMID] [PMCID]
- Rastegar S, Talebi S, Talebi S, Akbari M. [Comparison of the results of bandaging and casting in patients with first-and second-degree sprain of lateral ankle ligaments (Persian)]. Journal of Isfahan Medical School. 2017; 35(449):1321-6. [Link]
- Verhagen EA, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clinical Journal of Sport Medicine. 2000; 10(4):291-6. [DOI:10.1097/00042752-200010000-00012] [PMID]
- Garrick J, Requa R. The epidemiology of foot and ankle injuries in sports. Clinics in podiatric medicine and surgery. 1989; 6(3):629-37. [Link]
- Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, et al. Epidemiology of ankle arthritis: Report of a consecutive series of 639 patients from a tertiary orthopaedic center. The Iowa Orthopaedic Journal. 2005; 25:44. [PMCID]
- Peer KS, Barkley JE, Knapp DM. The acute effects of local vibration therapy on ankle sprain and hamstring strain injuries. The Physician and Sportsmedicine. 2009; 37(4):31-8. [DOI:10.3810/psm.2009.12.1739] [PMID]
- Almeida S, Williams K, Shaffer R, Brodine S. Epidemiological patterns of musculoskeletal injuries and physical training. Medicine & Science in Sports & Exercise. 1999; 31(8):1176-82. [DOI:10.1097/00005768-199908000-00015] [PMID]
Review Paper: Research |
Subject:
Special
Received: 2022/03/10 | Accepted: 2023/02/6 | Published: 2023/06/22
Received: 2022/03/10 | Accepted: 2023/02/6 | Published: 2023/06/22
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |