Volume 32, Issue 2 (7-2023)
JGUMS 2023, 32(2): 80-95 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salari A, Norouzi V, Naser Alavi F. Effect of Periodontitis and Periodontal Treatment on Positive Acute Phase Proteins. JGUMS 2023; 32 (2) :80-95
URL: http://journal.gums.ac.ir/article-1-2506-en.html
URL: http://journal.gums.ac.ir/article-1-2506-en.html
1- Department of Periodontics, Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran., Dental school of Rasht
2- Department of Periodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Operative Dentistry, Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran., Dental school of Rasht
2- Department of Periodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Operative Dentistry, Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran., Dental school of Rasht
Full-Text [PDF 7193 kb]
(650 Downloads)
| Abstract (HTML) (1564 Views)
Full-Text: (1454 Views)
Introduction
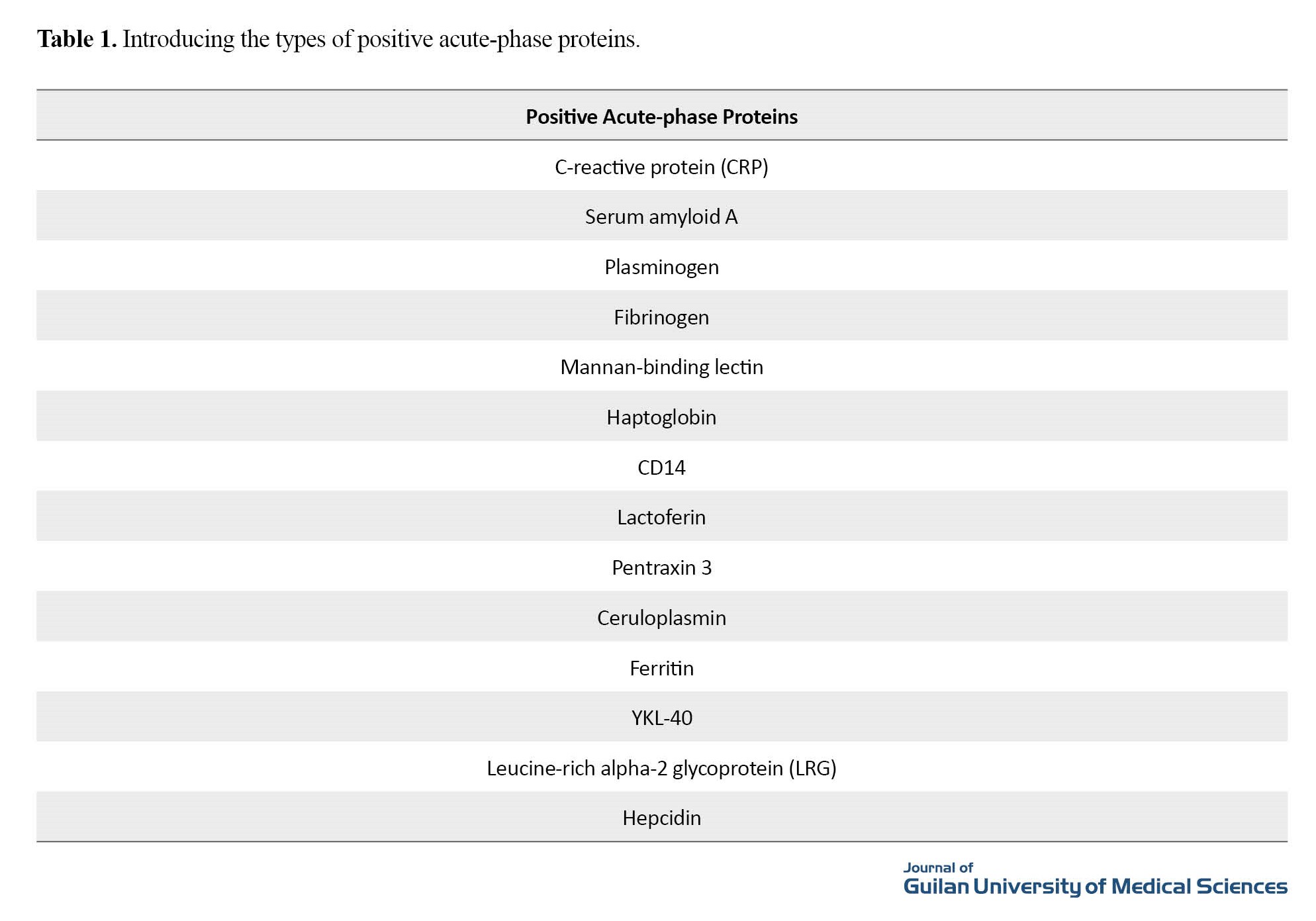
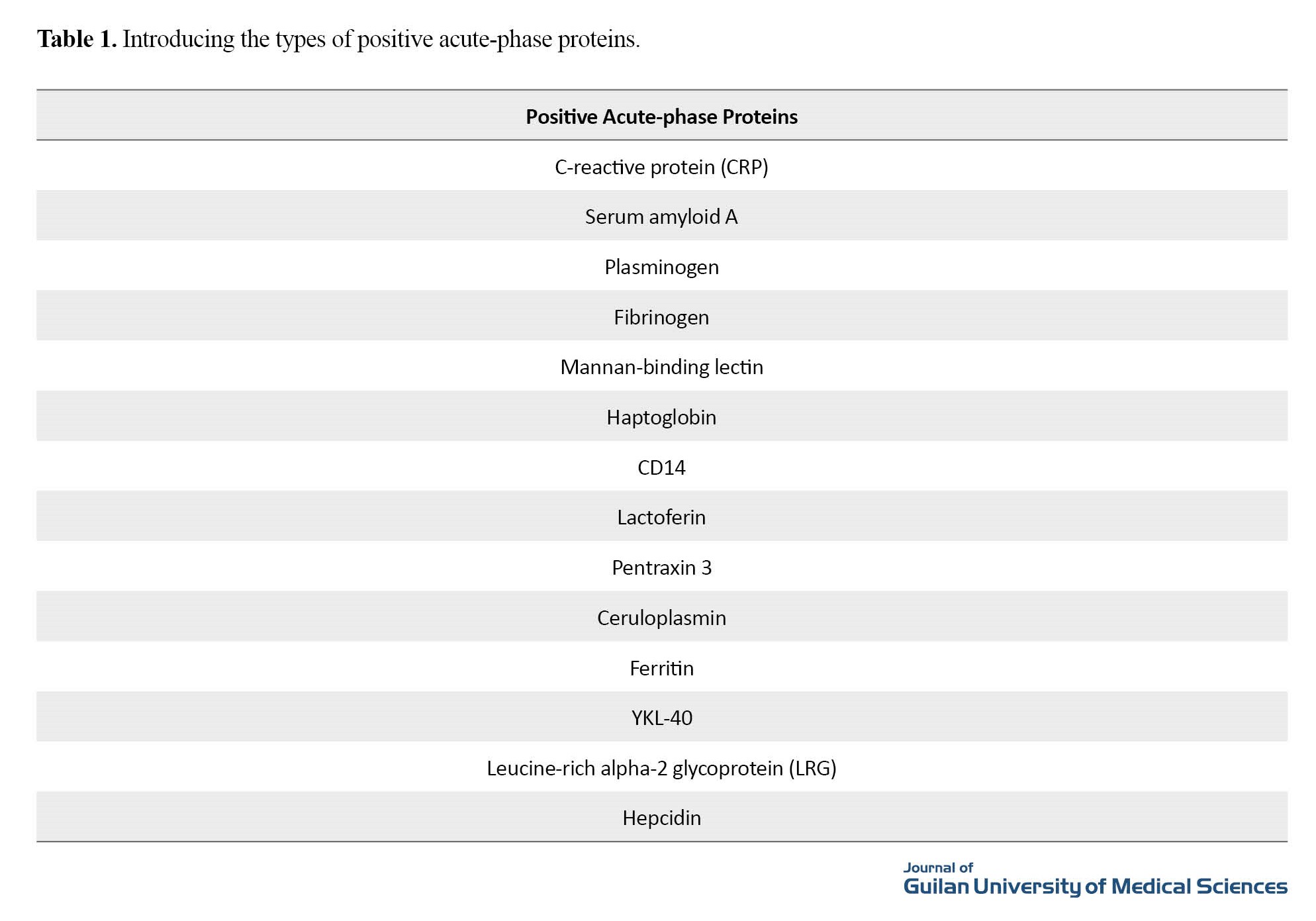
Periodontitis is an inflammatory-infectious disease caused by an imbalance between host defense mechanisms and specific periodontal pathogens and is associated with the long-term destruction of periodontal supporting tissues [1]. In this disease, gram-negative bacteria interact with the production of endotoxin in subgingival plaques by toll-like receptors (TLR) on the surface of polymorphonuclear leukocytes and monocytes. The complex, created by the interaction of endotoxins and TLR, activates the signal transduction pathway in both innate and acquired immunity, resulting in the production of cytokines that elicit local and systemic inflammatory responses. These inflammatory cytokines, which originate from the site of the disease, activate liver cells to produce acute-phase proteins (APPs) as part of a nonspecific response. APPs are a group of proteins that in response to inflammatory conditions (such as periodontal disease) the concentration of some of them increases (positive type) and the concentration of others (negative type) decreases (Table 1).
It is called the acute-phase response (APR) and occurs approximately 90 minutes after the onset of a systemic inflammatory reaction (Figure 1). Non-surgical periodontal treatment is usually the first step in the treatment process of periodontitis to eliminate its etiological agent and reduce inflammation and can change the concentration of inflammatory markers, such as APPs. The purpose of this review article was to investigate the types of APPs and the effect of inflammatory conditions in periodontitis and non-surgical periodontal treatment on them [2].
.jpg)
Methods
The present review was done to investigate the effect of inflammatory conditions, such as periodontal disease, and their treatment on the plasma levels of APPs. Articles were searched from 2000 to 2022 using the English keywords periodontitis, APPs, periodontal debridement, and inflammation mediators, separately and in combination. A preliminary search found 173 articles related to the effect of periodontal inflammatory disease on the level of APPs, of which 141 cases were found in Google Scholar and 32 in PubMed and Scopus. In the next step, articles were collected and initially reviewed, and studies with duplicate titles were removed. At this stage, the 56 articles had duplicate titles and were deleted. After checking the duplicates, the full text of the obtained studies was searched. Then, the abstract of the selected studies was reviewed based on the purpose of the review. Then, the final review and selection of studies based on the pre-defined inclusion and exclusion criteria were performed. These criteria included the time of publication, access to the original articles, and articles related to the effect of periodontitis and its treatment on the levels of APPs. Articles that were not in English or whose full text was not available or those that examined the effect of periodontitis on anything other than the positive type of acute-phase proteins were removed. The relevance of the articles was independently assessed by two researchers. Extraction of the required data was done using a pre-prepared checklist. Thus, another 52 articles were deleted and finally, 65 articles were selected and reviewed [1].
Results
From this review article, it can be concluded that periodontal disease as an inflammatory disease can lead to changes in the levels of APPs so that this disease leads to increased levels of these proteins and subsequently after periodontal treatment, a decrease is seen in their levels.
Discussion
Periodontitis is an inflammatory-infectious disease of the supporting tissues around the teeth, which if left untreated, leads to long-term destruction of these supporting tissues. In addition, it can lead to local and systemic inflammatory responses and subsequently change the levels of APPs. APPs, as a group of proteins that undergo changes in serum and plasma levels in response to inflammatory conditions, are divided into positive and negative types so that in inflammatory conditions, an increase in concentration is seen in the positive type and a decrease in concentration in the negative type.
A periodontal treatment includes non-surgical treatment, which is the first step in the treatment process, and its purpose is to remove etiological factors and reduce inflammation; thus, the gold standard in periodontal non-surgical treatment is scaling and root planing. After that, periodontal surgical treatment is performed to remove local and residual factors, if needed. After periodontal treatment, the concentration of positive APPs takes a reverse trend, and serum levels of positive APPs return to normal levels.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to preaparing the article.
Conflicts of interest
The authors declared that they have no competing interests with regard to authorship and/or publication of this paper.
References
Periodontitis is an inflammatory-infectious disease caused by an imbalance between host defense mechanisms and specific periodontal pathogens and is associated with the long-term destruction of periodontal supporting tissues [1]. In this disease, gram-negative bacteria interact with the production of endotoxin in subgingival plaques by toll-like receptors (TLR) on the surface of polymorphonuclear leukocytes and monocytes. The complex, created by the interaction of endotoxins and TLR, activates the signal transduction pathway in both innate and acquired immunity, resulting in the production of cytokines that elicit local and systemic inflammatory responses. These inflammatory cytokines, which originate from the site of the disease, activate liver cells to produce acute-phase proteins (APPs) as part of a nonspecific response. APPs are a group of proteins that in response to inflammatory conditions (such as periodontal disease) the concentration of some of them increases (positive type) and the concentration of others (negative type) decreases (Table 1).
It is called the acute-phase response (APR) and occurs approximately 90 minutes after the onset of a systemic inflammatory reaction (Figure 1). Non-surgical periodontal treatment is usually the first step in the treatment process of periodontitis to eliminate its etiological agent and reduce inflammation and can change the concentration of inflammatory markers, such as APPs. The purpose of this review article was to investigate the types of APPs and the effect of inflammatory conditions in periodontitis and non-surgical periodontal treatment on them [2].
.jpg)
Methods
The present review was done to investigate the effect of inflammatory conditions, such as periodontal disease, and their treatment on the plasma levels of APPs. Articles were searched from 2000 to 2022 using the English keywords periodontitis, APPs, periodontal debridement, and inflammation mediators, separately and in combination. A preliminary search found 173 articles related to the effect of periodontal inflammatory disease on the level of APPs, of which 141 cases were found in Google Scholar and 32 in PubMed and Scopus. In the next step, articles were collected and initially reviewed, and studies with duplicate titles were removed. At this stage, the 56 articles had duplicate titles and were deleted. After checking the duplicates, the full text of the obtained studies was searched. Then, the abstract of the selected studies was reviewed based on the purpose of the review. Then, the final review and selection of studies based on the pre-defined inclusion and exclusion criteria were performed. These criteria included the time of publication, access to the original articles, and articles related to the effect of periodontitis and its treatment on the levels of APPs. Articles that were not in English or whose full text was not available or those that examined the effect of periodontitis on anything other than the positive type of acute-phase proteins were removed. The relevance of the articles was independently assessed by two researchers. Extraction of the required data was done using a pre-prepared checklist. Thus, another 52 articles were deleted and finally, 65 articles were selected and reviewed [1].
Results
From this review article, it can be concluded that periodontal disease as an inflammatory disease can lead to changes in the levels of APPs so that this disease leads to increased levels of these proteins and subsequently after periodontal treatment, a decrease is seen in their levels.
Discussion
Periodontitis is an inflammatory-infectious disease of the supporting tissues around the teeth, which if left untreated, leads to long-term destruction of these supporting tissues. In addition, it can lead to local and systemic inflammatory responses and subsequently change the levels of APPs. APPs, as a group of proteins that undergo changes in serum and plasma levels in response to inflammatory conditions, are divided into positive and negative types so that in inflammatory conditions, an increase in concentration is seen in the positive type and a decrease in concentration in the negative type.
A periodontal treatment includes non-surgical treatment, which is the first step in the treatment process, and its purpose is to remove etiological factors and reduce inflammation; thus, the gold standard in periodontal non-surgical treatment is scaling and root planing. After that, periodontal surgical treatment is performed to remove local and residual factors, if needed. After periodontal treatment, the concentration of positive APPs takes a reverse trend, and serum levels of positive APPs return to normal levels.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to preaparing the article.
Conflicts of interest
The authors declared that they have no competing interests with regard to authorship and/or publication of this paper.
References
- upta S, Gupta I, Gupta R, BJ JA, Goswami A, Singh D. A comparative evaluation of serum CRP levels in chronic and aggressive periodontitis patients before and after non-surgical periodontal therapy-a clinical study. University Journal of Dental Sciences. 2020; 6(3):9-15. [DOI:10.21276/ujds.2020.6.3.2]
- Polepalle T, Moogala S, Boggarapu S, Pesala DS, Palagi FB. Acute phase proteins and their role in periodontitis: A review. Journal of Clinical and Diagnostic Research. 2015; 9(11):ZE01-5. [PMID] [PMCID] [DOI:10.7860/JCDR/2015/15692.6728]
- Górska R, Gregorek H, Kowalski J, Laskus-Perendyk A, Syczewska M, Madaliński K. Relationship between clinical parameters and cytokine profiles in inflamed gingival tissue and serum samples from patients with chronic periodontitis. Journal of Clinical Periodontology. 2003; 30(12):1046-52. [PMID]
- Lobão WJM, Carvalho RCC, Leite SAM, Rodrigues VP, Batista JE, Gomes-Filho IS, et al. Relationship between periodontal outcomes and serum biomarkers changes after non-surgical periodontal therapy. Anais da Academia Brasileira de Ciências. 2019; 91(2):e20170652. [PMID]
- Loos BG. Systemic markers of inflammation in periodontitis. Journal of Periodontology. 2005; 76(Suppl 11S):2106-15. [DOI:10.1902/jop.2005.76.11-S.2106]
- Marcaccini AM, Meschiari CA, Sorgi CA, Saraiva MC, de Souza AM, Faccioli LH, et al. Circulating interleukin-6 and high-sensitivity C-reactive protein decrease after periodontal therapy in otherwise healthy subjects. Journal of Periodontology. 2009; 80(4):594-602. [DOI:10.1902/jop.2009.080561] [PMID]
- Pradeep AR, Anuj S. Anemia of chronic disease and chronic periodontitis: does periodontal therapy have an effect on anemic status? Journal of Periodontology. 2011; 82(3):388-94. [PMID]
- Jacobsen S. Review of equine acute-phase proteins. Proceedings of the Annual Convention of the American Association of Equine Practitioners. 2007; 53:230-5. [Link]
- Walton RM, Cowell RL, Valenciano AC. Equine hematology, cytology, and clinical chemistry. New Jersey: John Wiley & Sons, Inc.; 2021. [DOI:10.1002/9781119500186]
- Chakraborty S, Tewari S, Sharma RK, Narula SC. Effect of non-surgical periodontal therapy on serum ferritin levels: an interventional study. Journal of Periodontology. 2014; 85(5):688-96. [PMID]
- Fitzsimmons TR, Sanders AE, Bartold PM, Slade GD. Local and systemic biomarkers in gingival crevicular fluid increase odds of periodontitis. Journal of Clinical Periodontology. 2010; 37(1):30-6. [PMID]
- Lu Q, Jin L. Human gingiva is another site of C-reactive protein formation. Journal of Clinical Periodontology. 2010; 37(9):789-96. [PMID]
- Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow JS. Acute-phase inflammatory response to periodontal disease in the US population. Journal of Dental Research. 2000; 79(1):49-57. [DOI:10.1177/00220345000790010] [PMID]
- Machado V, Botelho J, Escalda C, Hussain SB, Luthra S, Mascarenhas P, et al. Serum C-reactive protein and periodontitis: A systematic review and meta-analysis. Frontiers in Immunology. 2021; 12:706432. [DOI:10.3389/fimmu.2021.706432] [PMID] [PMCID]
- Luthra S, Grover HS, Singh A, Lall A, Masamatti SS. Comparative evaluation of C-reactive protein and complete blood count in chronic periodontitis patients following Phase I therapy: A serological and hematological study. Journal of Indian Society of Periodontology. 2019; 23(6):525-533. [DOI:10.4103/jisp.jisp_639_18] [PMID] [PMCID]
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. Journal of Periodontology. 2018; 89 (Suppl 1):S159-S72. [DOI:10.1002/JPER.18-0006] [PMID]
- Salzberg TN, Overstreet BT, Rogers JD, Califano JV, Best AM, Schenkein HA. C-reactive protein levels in patients with aggressive periodontitis. Journal of Periodontology. 2006; 77(6):933-9. [DOI:10.1902/jop.2006.050165] [PMID]
- Leite AC, Carneiro VM, Guimarães Mdo C. Effects of periodontal therapy on C-reactive protein and HDL in serum of subjects with periodontitis. Revista Brasileira de Cirurgia Cardiovascular. 2014; 29(1):69-77. [DOI:10.5935/1678-9741.20140013] [PMID] [PMCID]
- Jayaprakash D, Aghanashini S, Vijayendra RR, Chatterjee A, Rosh RM, Bharwani A. Effect of periodontal therapy on C-reactive protein levels in gingival crevicular fluid of patients with gingivitis and chronic periodontitis: A clinical and biochemical study. Journal of Indian Society of Periodontology. 2014; 18(4):456-60. [DOI:10.4103/0972-124X.138688] [PMID] [PMCID]
- Demmer RT, Trinquart L, Zuk A, Fu BC, Blomkvist J, Michalowicz BS, et al. The influence of anti-infective periodontal treatment on C-reactive protein: A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2013; 8(10):e77441. [DOI:10.1371/journal.pone.0077441] [PMID] [PMCID]
- Paraskevas S, Huizinga JD, Loos BG. A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. Journal of Clinical Periodontology. 2008; 35(4):277-90. [DOI:10.1111/j.1600-051X.2007.01173.x ] [PMID]
- Gruys E, Toussaint MJ, Niewold TA, Koopmans SJ. Acute phase reaction and acute phase proteins. Journal of Zhejiang University Science B. 2005; 6(11):1045-56. [PMID] [PMCID]
- Ardila CM, Guzmán IC. Comparison of serum amyloid A protein and C-reactive protein levels as inflammatory markers in periodontitis. Journal of Periodontal and Implant Science. 2015; 45(1):14-22. [DOI: https://doi.org/10.5051/jpis.2015.45.1.14] [PMID] [PMCID]
- Aoki-Nonaka Y, Nakajima T, Miyauchi S, Miyazawa H, Yamada H, Domon H, et al. Natural killer T cells mediate alveolar bone resorption and a systemic inflammatory response in response to oral infection of mice with Porphyromonas gingivalis. Journal of Periodontal Research. 2014; 49(1):69-76. [DOI:10.1111/jre.12080 PMID:23586756] [PMID]
- Graziani F, Cei S, La Ferla F, Vano M, Gabriele M, Tonetti M. Effects of non-surgical periodontal therapy on the glomerular filtration rate of the kidney: An exploratory trial. Journal of Clinical Periodontology. 2010; 37(7):638-43. [DOI:10.1111/j.1600-051X.2010.01578.x ] [PMID]
- Vuletic S, Taylor BA, Tofler GH, Chait A, Marcovina SM, Schenck K, et al. SAA and PLTP activity in plasma of periodontal patients before and after full-mouth tooth extraction. Oral Diseases. 2008; 14(6):514-9. [DOI:10.1111/j.1601-0825.2007.01411.x ] [PMID]
- Buduneli N, Buduneli E, Kardeşler L, Lappin D, Kinane DF. Plasminogen activator system in smokers and non-smokers with and without periodontal disease. Journal of Clinical Periodontology. 2005; 32(4):417-24. [PMID]
- Yin X, Bunn CL, Bartold PM. Detection of tissue plasminogen activator (t-PA) and plasminogen activator inhibitor 2 (PAI-2) in gingival crevicular fluid from healthy, gingivitis and periodontitis patients. Journal of Clinical Periodontology. 2000; 27(3):149-56. [10.1034/j.1600-051x.2000.027003149.x] [PMID]
- Wyganowska-Świątkowska M, Surdacka A, Skrzypczak-Jankun E, Jankun J. The plasminogen activation system in periodontal tissue (Review). International Journal of Molecular Medicine. 2014; 33(4):763-8. [PMID]
- Papadimitriou S, Tsantarliotou M, Makris G, Papaioannou N, Batzios Ch, Kokolis N, et al. A clinical study of plasminogen activator activity in gingival tissue in dogs with gingivitis and periodontitis. Research in Veterinary Science. 2006; 80(2):189-93. [DOI:10.1016/j.rvsc.2005.06.002] [PMID]
- Sahingur SE, Sharma A, Genco RJ, De Nardin E. Association of increased levels of fibrinogen and the -455G/A fibrinogen gene polymorphism with chronic periodontitis. Journal of Periodontology. 2003; 74(3):329-37. [DOI:10.1902/jop.2003.74.3.329] [PMID]
- Erickson HP. Size and shape of protein molecules at the nanometer level determined by sedimentation, gel filtration, and electron microscopy. Biological Procedures Online. 2009; 11:32-51. [PMID] [PMCID]
- Ana P, Draginja K, Dimitrije M, Ivan M, Mariola S. The markers of systemic inflammation in patients with chronic periodontitis: leukocytes, C-reactive protein and fibrinogen. World Journal of Preventive Medicine. 2013; 1(3):43-9. [Link]
- Chandy S, Joseph K, Sankaranarayanan A, Issac A, Babu G, Wilson B, et al. Evaluation of C-reactive protein and fibrinogen in patients with chronic and aggressive periodontitis: A clinico-biochemical study. Journal of Clinical and Diagnostic Research. 2017; 11(3):ZC41-5. [DOI:10.7860/JCDR/2017/23100.9552] [PMID] [PMCID]
- Tripathi VD. Estimation of fibrinogen and ESR-hemostatic markers in patients with mild, moderate and severe periodontitis. Indian Journal of Dental Sciences. 2014; 6(1):32-6. [Link]
- Maffei G, Brouwer N, Dolman KM, van der Velden U, Roos D, Loos BG. Plasma levels of mannan-binding lectin in relation to periodontitis and smoking. Journal of Periodontology. 2005; 76(11):1881-9. [DOI:10.1902/jop.2005.76.11.1881] [PMID]
- Tang H, Yuan C, Ma Z, Zhu C, Tong P, Gallagher JE, et al. The potentiality of salivary peptide biomarkers for screening patients with periodontal diseases by mass spectrometry. Clinical Chimica Acta. 2019; 495:278-86. [DOI:10.1016/j.cca.2019.04.076] [PMID]
- Kadkhodazadeh M, Ebadian AR, Tabari ZA, Amid R, Moscowchi A. Association of haptoglobin and natural resistance-associated macrophage protein 1 alleles with heme-consuming periodontal pathogens in chronic periodontitis and peri-implantitis: A pilot study. Journal of Advanced Periodontology & Implant Dentistry. 2020; 12(1):37-42. [DOI:10.34172/japid.2020.006] [PMID] [PMCID]
- Giannopoulou C, Cappuyns I, Cancela J, Cionca N, Mombelli A. Effect of photodynamic therapy, diode laser, and deep scaling on cytokine and acute-phase protein levels in gingival crevicular fluid of residual periodontal pockets. Journal of Periodontology. 2012; 83(8):1018-27. [DOI:10.1902/jop.2011.110281] [PMID]
- Haigh BJ, Stewart KW, Whelan JR, Barnett MP, Smolenski GA, Wheeler TT. Alterations in the salivary proteome associated with periodontitis. Journal of Clinical Periodontology. 2010; 37(3):241-7. [DOI:10.1111/j.1600-051X.2009.01525.x] [PMID]
- Nicu EA, Laine ML, Morré SA, Van der Velden U, Loos BG. Soluble CD14 in periodontitis. Innate Immunity. 2009; 15(2):121-8. [DOI:10.1177/1753425908101577] [PMID]
- Hirsch V, Blufstein A, Behm C, Andrukhov O. The alterations in CD14 expression in periodontitis: A systematic review. Applied Sciences. 2021; 11(5):2444. [DOI:10.3390/app11052444]
- Hayashi J, Masaka T, Ishikawa I. Increased levels of soluble CD14 in sera of periodontitis patients. Infection and Immunity. 1999; 67(1):417-20. [PMID] [PMCID]
- Arslan SY, Leung KP, Wu CD. The effect of lactoferrin on oral bacterial attachment. Oral Microbiology and Immunology. 2009; 24(5):411-6. [DOI:10.1111/j.1399-302X.2009.00537.x] [PMID]
- Glimvall P, Wickström C, Jansson H. Elevated levels of salivary lactoferrin, a marker for chronic periodontitis? Journal of Periodontal Research. 2012; 47(5):655-60. [DOI:10.1111/j.1600-0765.2012.01479.x] [PMID]
- Jentsch H, Sievert Y, Göcke R. Lactoferrin and other markers from gingival crevicular fluid and saliva before and after periodontal treatment. Journal of Clinical Periodontology. 2004; 31(7):511-4. [DOI:10.1111/j.1600-051X.2004.00512.x] [PMID]
- Berlutti F, Pilloni A, Pietropaoli M, Polimeni A, Valenti P. Lactoferrin and oral diseases: Current status and perspective in periodontitis. Annali di Stomatologia (Roma). 2011; 2(3-4):10-8. [PMCID]
- Adonogianaki E, Moughal NA, Kinane DF. Lactoferrin in the gingival crevice as a marker of polymorphonuclear leucocytes in periodontal diseases. Journal of Clinical Periodontology. 1993; 20(1):26-31. [DOI:10.1111/j.1600-051X.1993.tb01755.x] [PMID]
- Lakshmanan R, Jayakumar ND, Sankari M, Padmalatha O, Varghese S. Estimation of pentraxin-3 levels in the gingival tissues of chronic and aggressive periodontitis participants: An in vivo study. Journal of Periodontology. 2014; 85(2):290-7. [DOI:10.1902/jop.2013.120718] [PMID]
- Gümüş P, Nizam N, Nalbantsoy A, Özçaka Ö, Buduneli N. Saliva and serum levels of pentraxin-3 and interleukin-1β in generalized aggressive or chronic periodontitis. Journal of Periodontology. 2014; 85(3):e40-6 [DOI:10.1902/jop.2013.130281] [PMID]
- Pradeep AR, Kathariya R, Raghavendra NM, Sharma A. Levels of pentraxin-3 in gingival crevicular fluid and plasma in periodontal health and disease. Journal of Periodontology. 2011; 82(5):734-41. [DOI:10.1902/jop.2010.100526] [PMID]
- Fujita Y, Ito H, Sekino S, Numabe Y. Correlations between pentraxin 3 or cytokine levels in gingival crevicular fluid and clinical parameters of chronic periodontitis. Odontology. 2012; 100(2):215-21. [DOI:10.1007/s10266-011-0042-1] [PMID]
- Keles GC, Balli U, Cetinkaya BO, Ayas B, Findik A, Keles ZP, et al. Biochemical analysis of pentraxin 3 and fibrinogen levels in experimental periodontitis model. Mediators Inflamm. 2012; 2012:809801. [DOI:10.1155/2012/809801] [PMID] [PMCID]
- Harshavardhana B, Rath SK, Mukherjee M. Evaluation of serum ceruloplasmin in aggressive and chronic periodontitis patients. Journal of Indian Society of Periodontology. 2013; 17(3):333-7. [DOI:10.4103/0972-124X.115659] [PMID] [PMCID]
- Gupta P, Kumar A. Effects on serum ceruloplasmin levels before and after non-surgical periodontal therapy in patients with chronic periodontitis. Journal of Dental and Medical Sciences. 2020; 19(2):48-52. [Link]
- Mohammed AA, Youssef JM, Metwally SS, Anees MM. Evaluation of the serum ceruloplasmin level before and after non-surgical periodontal therapy in patients with chronic periodontitis. Stomatological Disease and Science. 2018; 2:3. [DOI:10.20517/2573-0002.2017.15]
- Faramarzi M, Sadighi M, Chitsazi M, Esmailzadeh M, Foladvand G. The effect of adjunctive use of melatonin as a supplement on serum ferritin level in periodontal patients: A randomized, controlled trial. Dental Research Journal. 2021; 18(1):39. [Link]
- Keles ZP, Keles GC, Avci B, Cetinkaya BO, Emingil G. Analysis of YKL-40 acute-phase protein and interleukin-6 levels in periodontal disease. Journal of Periodontology. 2014; 85(9):1240-6. [DOI:10.1902/jop.2014.130631] [PMID]
- Chavan V, Sabavath S, Babu CH, Boyapati L. Estimation of YKL-40 acute-phase protein in serum of patients with periodontal disease and healthy individuals: A clinical-biochemical study. Contemporary Clinical Dentistry. 2019; 10(2):249-55. [DOI:10.4103/ccd.ccd_471_18] [PMID] [PMCID]
- Kido J, Bando Y, Bando M, Kajiura Y, Hiroshima Y, Inagaki Y, et al. YKL-40 level in gingival crevicular fluid from patients with periodontitis and type 2 diabetes. Oral Diseases. 2015; 21(5):667-73. [DOI:10.1111/odi.12334] [PMID]
- Damodar S, Mehta DS. Effect of scaling and root planing on gingival crevicular fluid level of YKL-40 acute phase protein in chronic periodontitis patients with or without type 2 diabetes mellitus: A clinico-biochemical study. Journal of Indian Society of Periodontology. 2018; 22(1):40-44. [DOI:10.4103/jisp.jisp_95_17] [PMID] [PMCID]
- Keles Yucel ZP, Balli U. Leucine-rich alpha-2 glycoprotein (LRG): A novel acute phase protein expressed in Stage 3 Grade C periodontitis before and after periodontal therapy. Journal of Periodontology. 2021;9 2(1):104-12. [DOI:10.1002/JPER.20-0358] [PMID]
- Leite SAM, Casanovas RC, Rodrigues VP, Pereira AFV, Ferreira TCA, Nascimento FRFD, et al. The effect of nonsurgical periodontal therapy on hepcidin and on inflammatory and iron marker levels. Brazilian Oral Research. 2019; 33:e055. [DOI:10.1590/1807-3107bor-2019.vol33.0055] [PMID]
- Guo LN, Yang YZ, Feng YZ. Serum and salivary ferritin and Hepcidin levels in patients with chronic periodontitis and type 2 diabetes mellitus. BMC Oral Health. 2018; 18(1):63. [DOI:10.1186/s12903-018-0524-4] [PMID] [PMCID]
Review Paper: Research |
Subject:
Special
Received: 2022/06/7 | Accepted: 2023/01/9 | Published: 2023/06/22
Received: 2022/06/7 | Accepted: 2023/01/9 | Published: 2023/06/22
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









