Volume 32, Issue 3 (10-2023)
JGUMS 2023, 32(3): 194-205 |
Back to browse issues page
Research code: IR.GUMS.REC.1401.001
Ethics code: IR.GUMS.REC.1401.001
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ashobi M T, Samidoost P, Beghaei A, Ghazanfar Tehran S, Atarkar Roshan Z, Jafarinezhad A et al . The Frequency of Organ Donation and the Clinical Characteristics of Donors with Brain Death before and after the Outbreak of the COVID-19 Pandemic in Rasht, Iran. JGUMS 2023; 32 (3) :194-205
URL: http://journal.gums.ac.ir/article-1-2594-en.html
URL: http://journal.gums.ac.ir/article-1-2594-en.html
Mohammad Taghi Ashobi1 

 , Pirooz Samidoost2
, Pirooz Samidoost2 

 , Arin Beghaei3
, Arin Beghaei3 
 , Samaneh Ghazanfar Tehran3
, Samaneh Ghazanfar Tehran3 

 , Zahra Atarkar Roshan4
, Zahra Atarkar Roshan4 

 , Alireza Jafarinezhad5
, Alireza Jafarinezhad5 

 , Mohammad Sadegh Esmaeili Delshad *6
, Mohammad Sadegh Esmaeili Delshad *6 




 , Pirooz Samidoost2
, Pirooz Samidoost2 

 , Arin Beghaei3
, Arin Beghaei3 
 , Samaneh Ghazanfar Tehran3
, Samaneh Ghazanfar Tehran3 

 , Zahra Atarkar Roshan4
, Zahra Atarkar Roshan4 

 , Alireza Jafarinezhad5
, Alireza Jafarinezhad5 

 , Mohammad Sadegh Esmaeili Delshad *6
, Mohammad Sadegh Esmaeili Delshad *6 


1- Department of Surgery, Faculty of Medicine, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Surgery, Faculty of Medicine, Medical Education Research Center, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Anesthesiology Research Center, Department of Anesthesiology, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Social Medicine, Faculty of Medicine, Otolaryngology Research Center, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Internal Diseases, Faculty of Medicine, Inflammatory Lung Disease Research Center, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
6- Department of Vascular Surgery, Faculty of Medicine, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Surgery, Faculty of Medicine, Medical Education Research Center, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Anesthesiology Research Center, Department of Anesthesiology, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Social Medicine, Faculty of Medicine, Otolaryngology Research Center, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Internal Diseases, Faculty of Medicine, Inflammatory Lung Disease Research Center, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
6- Department of Vascular Surgery, Faculty of Medicine, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 4191 kb]
(652 Downloads)
| Abstract (HTML) (1717 Views)
Full-Text: (1252 Views)
Introduction
The world faced a critical new public health stressor with the emergence of SARS-CoV-2. Its spread was extraordinarily rapid, and in a matter of weeks countries across the world were affected, notably in their ability to manage health care needs [1, 2]. While many sectors of public structures were impacted by the pandemic, it particularly highlighted shortcomings in medical care infrastructures around the world that underscored the need to reorganize medical systems, as they were vastly unprepared and ill-equipped to manage a pandemic and simultaneously provide general and specialized medical care. This paper presents modalities in approaches to the pandemic by various countries, and the triaged reorganization of medical sections not considered first-line in the pandemic that was in many cases transformed into wards for treating COVID-19 cases. As new viruses and structural variants emerge, it is important to find solutions to streamline medical care in hospitals, which includes the expansion of digital network medicine (i.e. telemedicine and mobile health apps. Organ donation or organ transplantation rate was also affected by the COVID-19 pandemic. The World Health Organization (WHO) reported a decrease in organ donation and transplantation rates in many countries due to the pandemic, which had a significant impact on the lives of candidates for organ transplants. The pandemic affected the entire process of organ transplantation, from donor identification and assessment to organ retrieval, transportation, and transplantation [3, 4] due to infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The transplantation community has had to work together to develop new protocols and guidelines to ensure that organ transplantation can continue safely during the pandemic [5]. Northern Iran is one region that has been affected by the pandemic, and its impact on organ donation and transplantation in this region has not been well studied. Therefore, this study aims to address this gap in the literature by comparing the process of organ donation and transplantation before and after the COVID-19 pandemic in the transplant centers of northern Iran.
Methods
In this cross-sectional study, 75 patients with brain death who were sent to the transplant center of northern Iran in Rasht for organ donation from 2018 to 2021 were selected. Their various demographic and clinical characteristics, such as underlying disease, history of smoking and drug use, causes of brain death, type of donated organ, number of donated organs per patient, type of transplanted organ, and the location where the transplantation had been done. The study period was divided into two time periods: Before the pandemic (from July 2018 to February 2020) and during the pandemic (from February 2020 to August 2021). The data collected during these two periods were analyzed and compared to identify any significant difference. All data were collected by examining the medical records and interviewing family members of the deceased patients.
Results
In the present study, the majority of organ donors were male aged 51-60 years (mean age: 37.40±16.32 years). About 65.3% were from urban areas; 66.10% had a history of smoking; 32% had underlying diseases. The most common underlying diseases was hypertension. Trauma (52%) and cerebrovascular disease (36%) were the most common causes of brain death. the most common type of trauma led to brain death was road accidents (45.3%). The most common cerebrovascular diseases led to brain death were intracerebral hemorrhage due to high blood pressure and brain aneurysm rupture. Of 75 patients, 43 had donated organs before the pandemic and 32 during the pandemic. A total of 167 abdominal organs (67 livers and 100 kidneys) had been donated (Table 1).
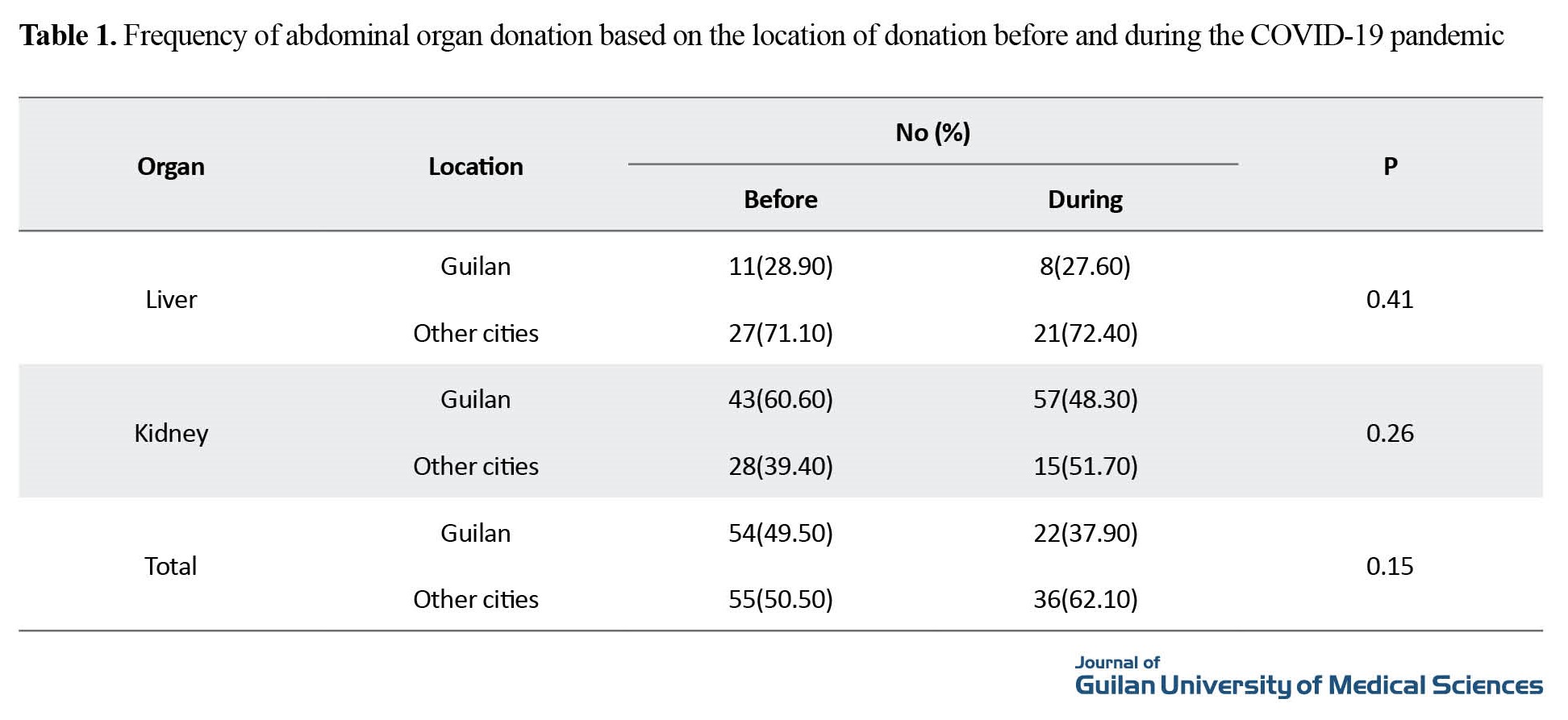
Comparison based on the demographic and clinical characteristics of deceased abdominal organ donors before and after the COVID-19 pandemic showed a statistically significant in age; the donors during the pandemic were older than those donated before the pandemic. There was no statistically significant difference in terms of smoking and opium use (P=0.61). Although the percentage of donors with underlying diseases was higher during the pandemic than before the pandemic (43% vs 23%), the difference was not statistically significant (P=0.06). A significant difference was found in the cause of brain death before and during the pandemic (P=0.015). The most common cause of brain death before the pandemic was trauma, while after the pandemic it was cerebrovascular diseases. There was a significant difference in the mean number of donated organs per each patient before and during the pandemic (P<0.001). However, there was no significant difference in the location of organ donation before and during the pandemic (P>0.05).
Conclusion
The results of this study showed that the COVID-19 pandemic had a significant impact on the process of organ donation and transplantation in the northern Iran. In comparing the two time periods of before and after the COVID-19 outbreak, a statistically significant difference was found in the mean number of donated organs per patient. The decrease in the number of donated organs during the pandemic can be attributed to several factors such as the fear of contracting the virus, restrictions in traveling, and the closure of some hospitals and medical centers.
Another finding of this study was the significant difference in the causes of brain death in donors before and during the COVID-19 pandemic. The most common cause of brain death before the pandemic was trauma, while after the pandemic, cerebrovascular diseases were the leading cause. This result can be attributed to the fact that COVID-19 is known to cause coagulation disorders, which increase the risk of cerebrovascular diseases. Furthermore, the results of this study showed that the pandemic had no significant effect on the type of transplanted organs and the location of transplantation (in or out of Guilan Province). This finding suggests that the pandemic had a more significant impact on the availability of organs rather than the transplantation process itself.
The findings of this study can be useful in planning to ensure the continuity of organ transplantation programs in future pandemics. Strategies such as increasing the public awareness and addressing fears related to organ donation, implementing safety measures to protect both patients and healthcare workers, and ensuring the availability of medical centers for transplantation can be effective in maintaining the continuity of organ transplantation programs during the pandemics.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.001).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and study design: Mohammad Taghi Ashoobi, Pirooz Shamidoost, and Mohammad Sadegh Esmaeili Delshad; Data acquisition and data analysis: Arian Baghaei, Samaneh Ghazanfar Tehran, and Zara Atrkar Roushan; Statistical analysis: Zara Atrkar Roushan and Arian Baghaei; Drafting of the manuscript and administrative, technical support: Alireza Jafarinezhad and Pirooz Shamidoost; Critical revision of the manuscript for important intellectual content: Mohammad Taghi Ashoobi, Mohammad Sadegh Esmaeili Delshad, and Samaneh Ghazanfar Tehran; Funding acquisition and supervision: Mohammad Taghi Ashoobi and Mohammad Sadegh Esmaeili Delshad.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all medical staff of Razi Hospital for their cooperation in this study.
References
The world faced a critical new public health stressor with the emergence of SARS-CoV-2. Its spread was extraordinarily rapid, and in a matter of weeks countries across the world were affected, notably in their ability to manage health care needs [1, 2]. While many sectors of public structures were impacted by the pandemic, it particularly highlighted shortcomings in medical care infrastructures around the world that underscored the need to reorganize medical systems, as they were vastly unprepared and ill-equipped to manage a pandemic and simultaneously provide general and specialized medical care. This paper presents modalities in approaches to the pandemic by various countries, and the triaged reorganization of medical sections not considered first-line in the pandemic that was in many cases transformed into wards for treating COVID-19 cases. As new viruses and structural variants emerge, it is important to find solutions to streamline medical care in hospitals, which includes the expansion of digital network medicine (i.e. telemedicine and mobile health apps. Organ donation or organ transplantation rate was also affected by the COVID-19 pandemic. The World Health Organization (WHO) reported a decrease in organ donation and transplantation rates in many countries due to the pandemic, which had a significant impact on the lives of candidates for organ transplants. The pandemic affected the entire process of organ transplantation, from donor identification and assessment to organ retrieval, transportation, and transplantation [3, 4] due to infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The transplantation community has had to work together to develop new protocols and guidelines to ensure that organ transplantation can continue safely during the pandemic [5]. Northern Iran is one region that has been affected by the pandemic, and its impact on organ donation and transplantation in this region has not been well studied. Therefore, this study aims to address this gap in the literature by comparing the process of organ donation and transplantation before and after the COVID-19 pandemic in the transplant centers of northern Iran.
Methods
In this cross-sectional study, 75 patients with brain death who were sent to the transplant center of northern Iran in Rasht for organ donation from 2018 to 2021 were selected. Their various demographic and clinical characteristics, such as underlying disease, history of smoking and drug use, causes of brain death, type of donated organ, number of donated organs per patient, type of transplanted organ, and the location where the transplantation had been done. The study period was divided into two time periods: Before the pandemic (from July 2018 to February 2020) and during the pandemic (from February 2020 to August 2021). The data collected during these two periods were analyzed and compared to identify any significant difference. All data were collected by examining the medical records and interviewing family members of the deceased patients.
Results
In the present study, the majority of organ donors were male aged 51-60 years (mean age: 37.40±16.32 years). About 65.3% were from urban areas; 66.10% had a history of smoking; 32% had underlying diseases. The most common underlying diseases was hypertension. Trauma (52%) and cerebrovascular disease (36%) were the most common causes of brain death. the most common type of trauma led to brain death was road accidents (45.3%). The most common cerebrovascular diseases led to brain death were intracerebral hemorrhage due to high blood pressure and brain aneurysm rupture. Of 75 patients, 43 had donated organs before the pandemic and 32 during the pandemic. A total of 167 abdominal organs (67 livers and 100 kidneys) had been donated (Table 1).
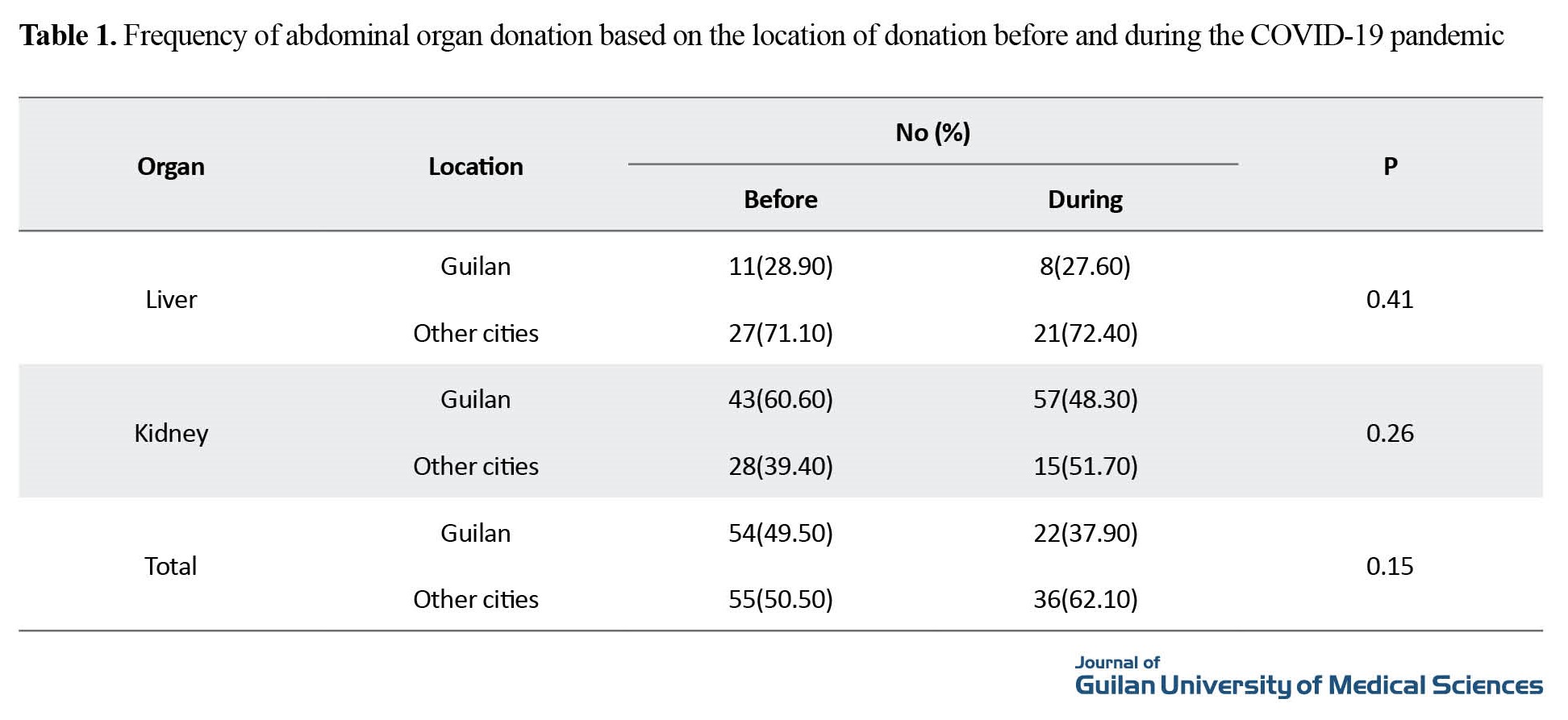
Comparison based on the demographic and clinical characteristics of deceased abdominal organ donors before and after the COVID-19 pandemic showed a statistically significant in age; the donors during the pandemic were older than those donated before the pandemic. There was no statistically significant difference in terms of smoking and opium use (P=0.61). Although the percentage of donors with underlying diseases was higher during the pandemic than before the pandemic (43% vs 23%), the difference was not statistically significant (P=0.06). A significant difference was found in the cause of brain death before and during the pandemic (P=0.015). The most common cause of brain death before the pandemic was trauma, while after the pandemic it was cerebrovascular diseases. There was a significant difference in the mean number of donated organs per each patient before and during the pandemic (P<0.001). However, there was no significant difference in the location of organ donation before and during the pandemic (P>0.05).
Conclusion
The results of this study showed that the COVID-19 pandemic had a significant impact on the process of organ donation and transplantation in the northern Iran. In comparing the two time periods of before and after the COVID-19 outbreak, a statistically significant difference was found in the mean number of donated organs per patient. The decrease in the number of donated organs during the pandemic can be attributed to several factors such as the fear of contracting the virus, restrictions in traveling, and the closure of some hospitals and medical centers.
Another finding of this study was the significant difference in the causes of brain death in donors before and during the COVID-19 pandemic. The most common cause of brain death before the pandemic was trauma, while after the pandemic, cerebrovascular diseases were the leading cause. This result can be attributed to the fact that COVID-19 is known to cause coagulation disorders, which increase the risk of cerebrovascular diseases. Furthermore, the results of this study showed that the pandemic had no significant effect on the type of transplanted organs and the location of transplantation (in or out of Guilan Province). This finding suggests that the pandemic had a more significant impact on the availability of organs rather than the transplantation process itself.
The findings of this study can be useful in planning to ensure the continuity of organ transplantation programs in future pandemics. Strategies such as increasing the public awareness and addressing fears related to organ donation, implementing safety measures to protect both patients and healthcare workers, and ensuring the availability of medical centers for transplantation can be effective in maintaining the continuity of organ transplantation programs during the pandemics.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1401.001).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and study design: Mohammad Taghi Ashoobi, Pirooz Shamidoost, and Mohammad Sadegh Esmaeili Delshad; Data acquisition and data analysis: Arian Baghaei, Samaneh Ghazanfar Tehran, and Zara Atrkar Roushan; Statistical analysis: Zara Atrkar Roushan and Arian Baghaei; Drafting of the manuscript and administrative, technical support: Alireza Jafarinezhad and Pirooz Shamidoost; Critical revision of the manuscript for important intellectual content: Mohammad Taghi Ashoobi, Mohammad Sadegh Esmaeili Delshad, and Samaneh Ghazanfar Tehran; Funding acquisition and supervision: Mohammad Taghi Ashoobi and Mohammad Sadegh Esmaeili Delshad.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all medical staff of Razi Hospital for their cooperation in this study.
References
- Abbasi P, Yoosefi Lebni J, Nouri P, Ziapour A, Jalali A. The obstacles to organ donation following brain death in Iran: A qualitative study. BMC Medical Ethics. 2020; 21(1):83. [DOI:10.1186/s12910-020-00529-8] [PMID] [PMCID]
- Ríos A, López-Navas A, López-López A, Gómez FJ, Iriarte J, Herruzo R, et al. A multicentre and stratified study of the attitude of medical students towards organ donation in Spain. Ethnicity & Health. 2019; 24(4):443-61. [DOI:10.1080/13557858.2017.1346183] [PMID]
- Krupic F. The impact of religion and provision of information on increasing knowledge and changing attitudes to organ donation: An intervention study. Journal of Religion and Health. 2020; 59(4):2082-95. [DOI:10.1007/s10943-019-00961-0] [PMID] [PMCID]
- Stadlbauer V, Zink C, Likar P, Zink M. Family discussions and demographic factors influence adolescent's knowledge and attitude towards organ donation after brain death: A questionnaire study. BMC Medical Ethics. 2020; 21(1):57. [DOI:10.1186/s12910-020-00499-x] [PMID] [PMCID]
- Parsa P, Taheri M, Rezapur-Shahkolai F, Shirahmadi S. Attitudes of Iranian students about organ donation: A qualitative study. BMC Medical Ethics. 2019; 20(1):36. [DOI:10.1186/s12910-019-0372-z] [PMID] [PMCID]
- Baj J, Karakuła-Juchnowicz H, Teresiński G, Buszewicz G, Ciesielka M, Sitarz R, et al. COVID-19: Specific and non-specific clinical manifestations and symptoms: The current state of knowledge. Journal of Clinical Medicine. 2020; 9(6):1753. [DOI:10.3390/jcm9061753] [PMID] [PMCID]
- Zhang BH, Yan LN, Yang JY. Organ transplantation management in the midst of the COVID-19 outbreak: A synopsis. Hepatobiliary Surgery and Nutrition. 2020; 9(2):250-2. [DOI:10.21037/hbsn.2020.03.16] [PMID] [PMCID]
- Kumar D, Manuel O, Natori Y, Egawa H, Grossi P, Han SH, et al. COVID-19: A global transplant perspective on successfully navigating a pandemic. American Journal of Transplantation. 2020; 20(7):1773-9. [DOI:10.1111/ajt.15876] [PMID] [PMCID]
- Ali Malekhosseini S, Nikoupour H, Gholami S, Shamsaeefar A, Arasteh P, Kazemi K, et al. A report of 85 cases of COVID-19 and abdominal transplantation from a single center: What are the associated factors with death among organ transplantation patients. Transplantation. 2021; 105(1):90-9. [DOI:10.1097/TP.0000000000003470] [PMID]
- Moris D, Shaw BI, Dimitrokallis N, Barbas AS. Organ donation during the coronavirus pandemic: An evolving saga in uncharted waters. Transplant International. 2020; 33(7):826-7. [DOI:10.1111/tri.13614] [PMID] [PMCID]
- Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020; 158(6):1831-3. [DOI:10.1053/j.gastro.2020.02.055] [PMID] [PMCID]
- Akpeke H, Dzando G, Kumah A, Keronei D, Bimba Donyi A, Salifu S, et al. Health policy and the fight against COVID-19: A narrative review of Ghana’s Response. Health in Emergencies and Disasters Quarterly. 2022; 7(3):101–8. [Link]
- Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, Jacquelinet C. Organ procurement and transplantation during the COVID-19 pandemic. Lancet. 2020; 395(10237):e95-6. [DOI:10.1016/S0140-6736(20)31040-0] [PMID]
- Aubert O, Yoo D, Zielinski D, Cozzi E, Cardillo M, Dürr M, et al. COVID-19 pandemic and worldwide organ transplantation: A population-based study. The Lancet. Public Health. 2021; 6(10):e709-19.[DOI:10.1016/S2468-2667(21)00200-0] [PMID]
- Iranian Society of Organ Donation. [Organ donation statistics 2020 (Persian)]. Tehran: Iranian Society of Organ Donation; 2020. [Link]
- Latifi M, Bagherpour F, Jafarian A, Hamidiyeh A, Javandoost E, Mansouri Z, et al. Evaluating the impact of COVID-19 pandemic on organ donation and transplantation activities in Iran. Shiraz E-Medical Journal. 2022; 23(1):e116048. [DOI:10.5812/semj.116048] [PMID]
- Mokhber Dezfuli M, Eslami F, Mostafavi K, Khoshkholgh R, Reza Nejatollahi SM, Montazeri S, et al. Organ procurement from donors after brain death during the COVID-19 pandemic: Experience of a high prevalence country. Experimental and Clinical Transplantation. 2022; 20(4):420-4. [DOI:10.6002/ect.2021.0398] [PMID]
- Manara AR, Mumford L, Callaghan CJ, Ravanan R, Gardiner D. Donation and transplantation activity in the UK during the COVID-19 lockdown. Lancet. 2020; 396(10249):465-6. [DOI:10.1016/S0140-6736(20)31692-5] [PMID]
- Raoofi A, Takian A, Akbari Sari A, Olyaeemanesh A, Haghighi H, Aarabi M. COVID-19 pandemic and comparative health policy learning in Iran. Archives of Iranian Medicine. 2020; 23(4):220-34. [DOI:10.34172/aim.2020.02] [PMID]
- Cheung CY, Pong ML, Au Yeung SF, Chak WL. Impact of COVID-19 pandemic on organ donation in Hong Kong: A single-center observational study. Transplantation Proceedings. 2021; 53(4):1143-5. [DOI:10.1016/j.transproceed.2021.02.016] [PMID] [PMCID]
- Qu Z, Oedingen C, Bartling T, Schrem H, Krauth C. Organ procurement and transplantation in Germany during the COVID-19 pandemic. Lancet. 2020; 396(10260):1395. [DOI:10.1016/S0140-6736(20)32213-3] [PMID]
- Rimaz S, Panahi L, Pouy S. Organ procurement and transplantation during the COVID-19 pandemic in Iran. Korean Journal of Transplantation. 2022; 36(1):79-80. [DOI:10.4285/kjt.21.0032] [PMID] [PMCID]
- Michel S, Witt C, Gottlieb J, Aigner C. Impact of COVID-19 on lung transplant activity in Germany-A cross-sectional survey. The Thoracic and Cardiovascular Surgeon. 2021; 69(1):92-4.[DOI:10.1055/s-0040-1715436] [PMID]
- Picard C, Le Pavec J, Tissot A; Groupe Transplantation Pulmonaire de la Société de Pneumologie de Langue Française SPLF. Impact of the COVID-19 pandemic and lung transplantation program in France. Respiratory Medicine and Research. 2020; 78:100758. [DOI:10.1016/j.resmer.2020.100758] [PMID] [PMCID]
Review Paper: Research |
Subject:
General
Received: 2023/02/8 | Accepted: 2023/07/8 | Published: 2023/10/1
Received: 2023/02/8 | Accepted: 2023/07/8 | Published: 2023/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |