Volume 34, Issue 1 (3-2025)
JGUMS 2025, 34(1): 70-79 |
Back to browse issues page
Research code: 2595
Ethics code: 1401.160
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
mahfoozi L, haghighi M, Rezaei S, karimian P. The Relationship of Some Liver Function Tests and Red Blood Cell Parameters With Disease Outcome of Patients With COVID-19 Admitted to Razi Hospital, Rasht, Northern Iran. JGUMS 2025; 34 (1) :70-79
URL: http://journal.gums.ac.ir/article-1-2615-en.html
URL: http://journal.gums.ac.ir/article-1-2615-en.html
1- Department of Infectious Disease, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Anesthesiology, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- Inflammatory Lung Diseases Research Center, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Pathology, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Anesthesiology, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- Inflammatory Lung Diseases Research Center, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Pathology, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 3250 kb]
(232 Downloads)
| Abstract (HTML) (1034 Views)
Full-Text: (299 Views)
Introduction
COVID-19 caused a wide range of clinical symptoms, the most common of which were fever, dry cough, and fatigue [3, 4]. Severe cases led to severe pneumonia, respiratory and multi-organ failure, and ultimately death [5]. Liver function test (LFT) abnormalities are seen in 14-53% of patients as abnormal levels of aspartate transaminase (AST), alanine transaminase (ALT), mild elevation of bilirubin and prolonged prothrombin time (PT) [6, 7, 8]. Elevations in cholestatic markers and AST were observed more frequently compared to ALT. These abnormalities were significantly higher and more common in patients with severe COVID-19 than in other patients [10, 11] and can be an independent predictor of transfer to the intensive care unit (ICU), disease complications and death [12]. A study of liver autopsies from 48 patients with severe COVID-19 showed significant vascular thrombosis with steatosis, hydronephrosis, lobular inflammation and portal fibrosis. This liver injury could occur through various mechanisms [9, 13, 14]. In patients with severe forms of the disease, changes in hematological test results, such as a significant increase in white blood cell count, a decrease in platelets, and lymphopenia, had been frequently observed [15]. Moreover, a correlation was observed between hemoglobin (Hb) levels at admission and disease progression in COVID-19 patients, with lower hemoglobin levels being associated with more severe disease progression and higher mortality. During hospitalization, the incidence of anemia was 65% in COVID-19 patients admitted to the ICU and 43% in other patients [17, 18]. Studies on the association of some LFTs and red blood cell parameters with the final outcome (recovery versus death) in COVID-19 patients, especially in Iran, have been limited. Therefore, this study aimed to investigate the relationship between some laboratory factors, such as LFTs and red blood cell parameters, and the outcome of patients with COVID-19 hospitalized at Razi Hospital in Rasht, northern Iran.
Methods
This cross-sectional analytical study was conducted on patients with COVID-19 hospitalized at Razi Hospital in Rasht, northern Iran, during 2021, whose COVID-19 was confirmed by RT-PCR testing. Using a convenience sampling method, 195 were included in the study. Demographic information and some red blood cell parameters, including Hb, HCT, MCV and some LFTs such as AST, ALT, ALKP, Total bilirubin and PT, were recorded from the patient’s file. Patient outcomes were recovery or discharge from the hospital, death, and length of hospitalization. Mean±SD were used to describe quantitative variables and frequency and percentage were used to describe qualitative variables. Shapiro-Wilk test was used to check the normality of the data. Mann-Whitney U test and Spearman correlation test were used to examine the relationship between quantitative variables. The significance level was set at 0.05.
Results
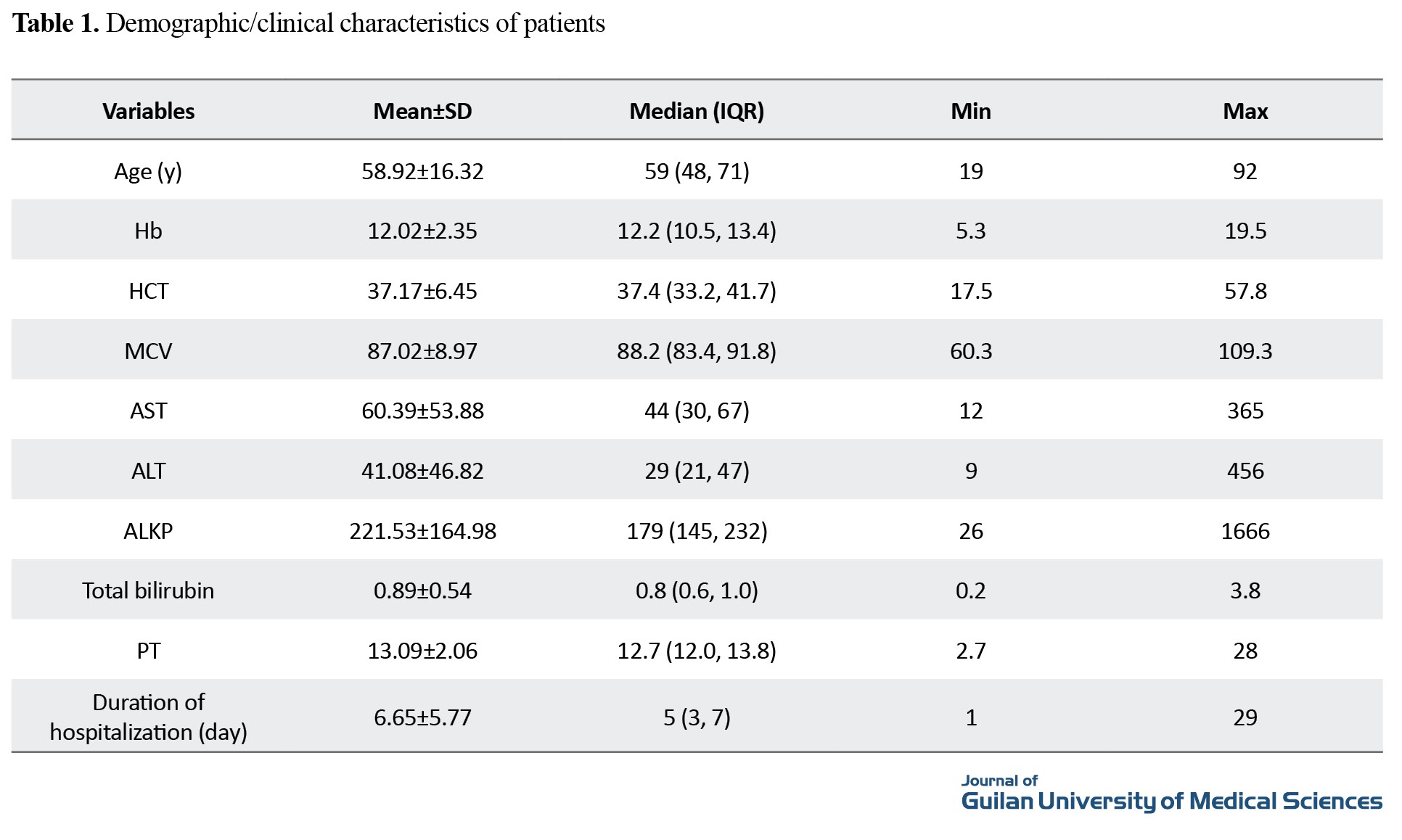
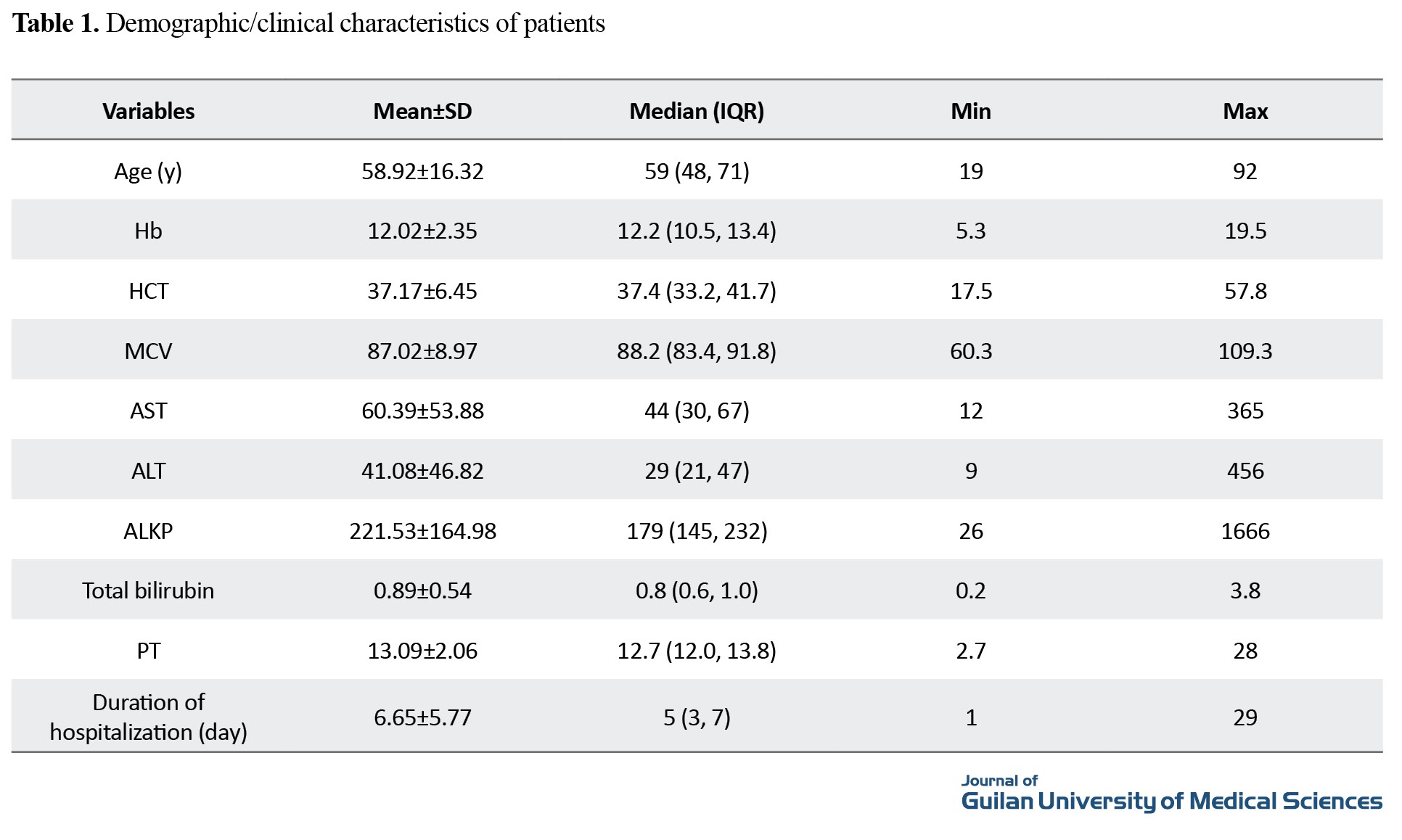
In this study, the mean age of the patients was 58.92±16.39 years. Of 195 patients, 106(54.4%) were female, and 89(45.6%) were male. The demographic and clinical information of the patients is reported in Table 1.
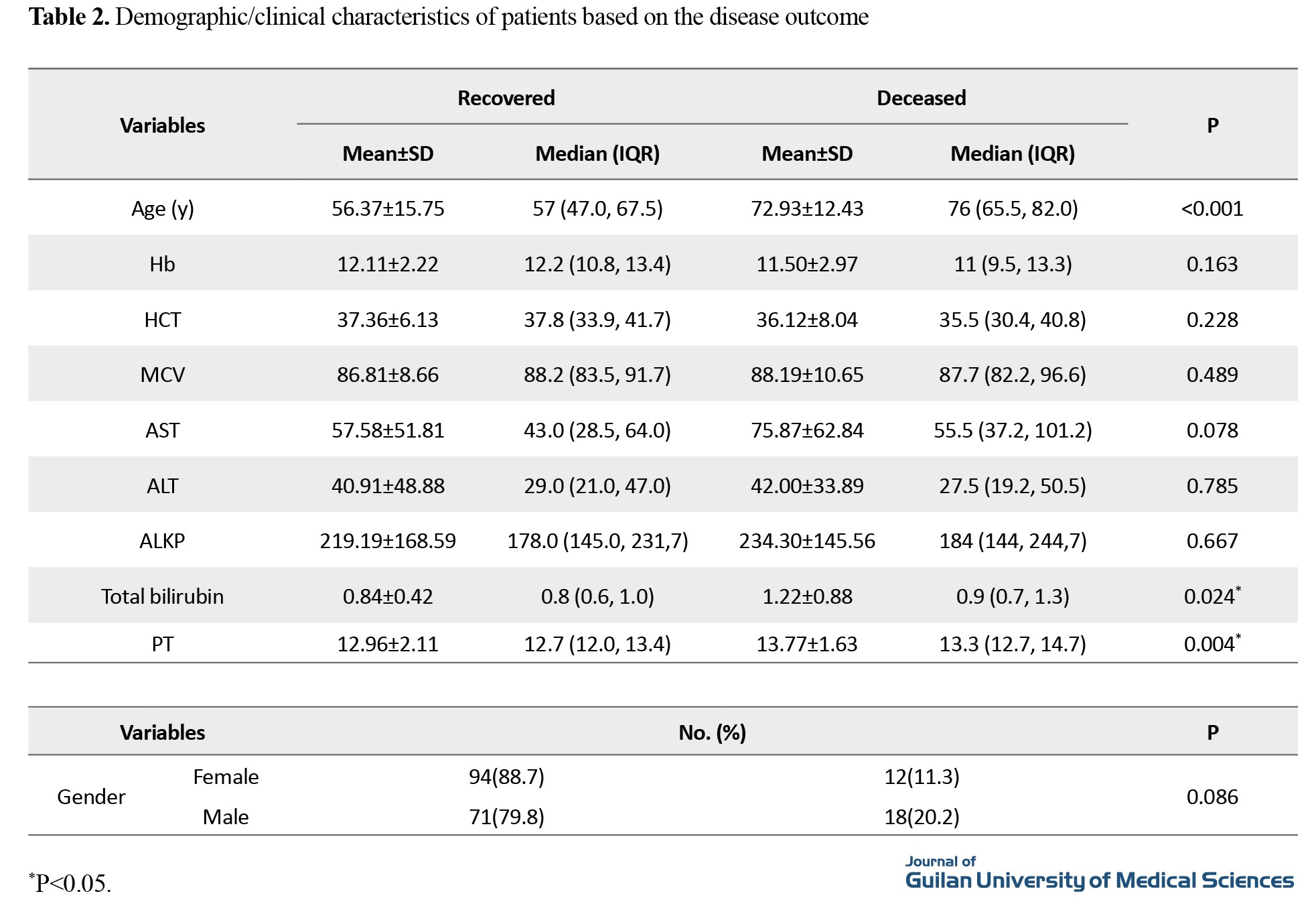
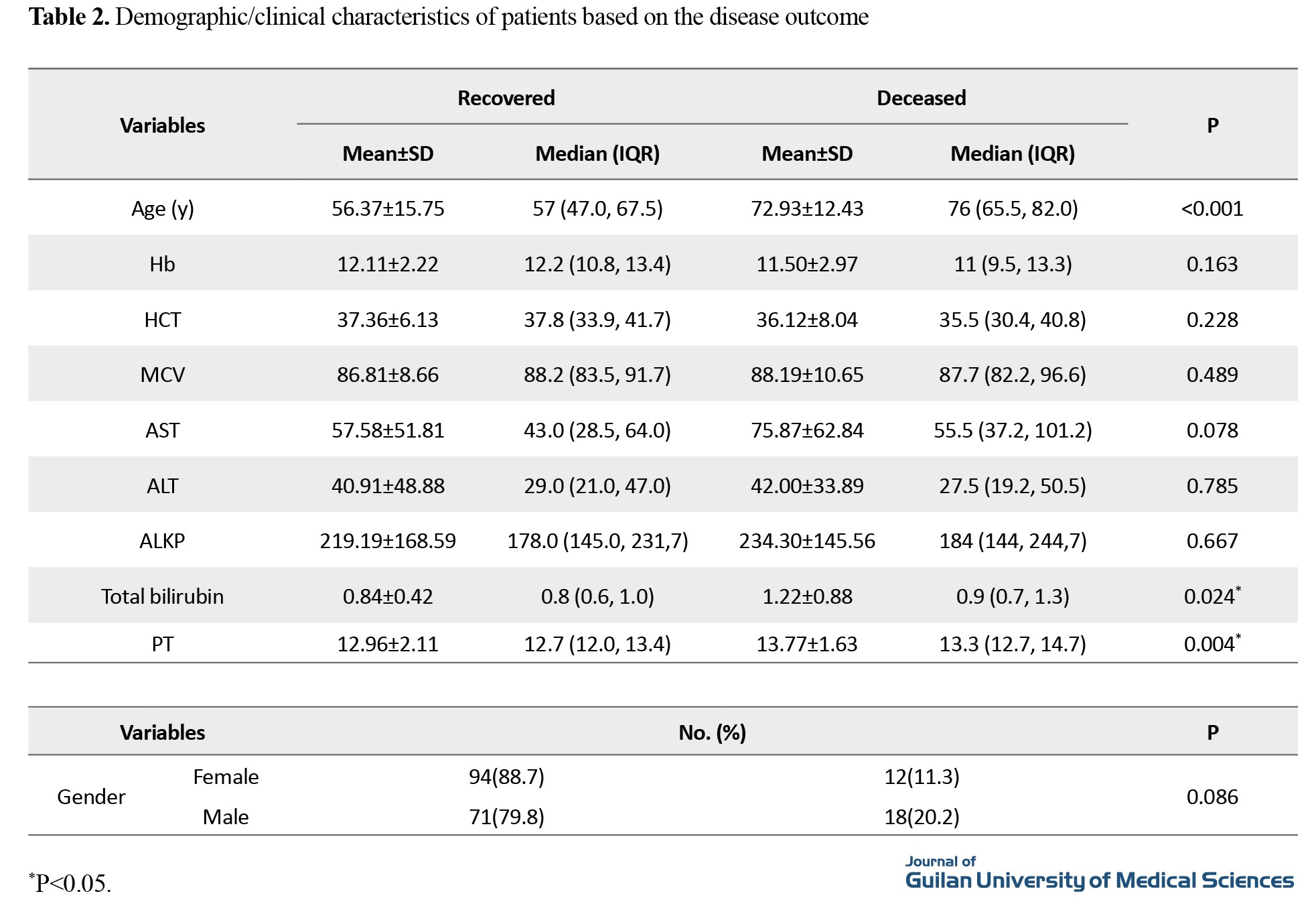
Mortality was observed in 15.4% of cases (n=30), and recovery in 84.6% (n=165). None of the data had a normal distribution. The results of examining the relationship between the studied factors and the outcome of patients are reported in Table 2.
Conclusion
Overall, the findings of this study showed that age, total bilirubin, and PT are the risk factors associated with the outcome of COVID-19 patients. Also, low levels of Hb and HCT are associated with prolonged hospitalization. There is no significant association between liver enzyme parameters of ALT and AST and the outcome of patients with COVID-19. It is recommended that other prospective studies, if possible, be designed and implemented using a larger sample size and other laboratory parameters, paying attention to their impact on long-term complications in COVID-19 patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1401.160).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualizing, and methodology: Lida Mahfoozi; Validation and analysis: Mohammad Haghighi; Investigation and writing the original draft: Sepinood Rezaei; Review and editing, and project management: Paridokht Karimian Supervision: Lida Mahfoozi and Paridokht Karimian.
Conflicts of interest
The authors declared that there are no conflicts of interest in this article.
Acknowledgements
The authors would like to express their gratitude to the medical staff of Razi Hospital, Rasht, Iran.
References
COVID-19 caused a wide range of clinical symptoms, the most common of which were fever, dry cough, and fatigue [3, 4]. Severe cases led to severe pneumonia, respiratory and multi-organ failure, and ultimately death [5]. Liver function test (LFT) abnormalities are seen in 14-53% of patients as abnormal levels of aspartate transaminase (AST), alanine transaminase (ALT), mild elevation of bilirubin and prolonged prothrombin time (PT) [6, 7, 8]. Elevations in cholestatic markers and AST were observed more frequently compared to ALT. These abnormalities were significantly higher and more common in patients with severe COVID-19 than in other patients [10, 11] and can be an independent predictor of transfer to the intensive care unit (ICU), disease complications and death [12]. A study of liver autopsies from 48 patients with severe COVID-19 showed significant vascular thrombosis with steatosis, hydronephrosis, lobular inflammation and portal fibrosis. This liver injury could occur through various mechanisms [9, 13, 14]. In patients with severe forms of the disease, changes in hematological test results, such as a significant increase in white blood cell count, a decrease in platelets, and lymphopenia, had been frequently observed [15]. Moreover, a correlation was observed between hemoglobin (Hb) levels at admission and disease progression in COVID-19 patients, with lower hemoglobin levels being associated with more severe disease progression and higher mortality. During hospitalization, the incidence of anemia was 65% in COVID-19 patients admitted to the ICU and 43% in other patients [17, 18]. Studies on the association of some LFTs and red blood cell parameters with the final outcome (recovery versus death) in COVID-19 patients, especially in Iran, have been limited. Therefore, this study aimed to investigate the relationship between some laboratory factors, such as LFTs and red blood cell parameters, and the outcome of patients with COVID-19 hospitalized at Razi Hospital in Rasht, northern Iran.
Methods
This cross-sectional analytical study was conducted on patients with COVID-19 hospitalized at Razi Hospital in Rasht, northern Iran, during 2021, whose COVID-19 was confirmed by RT-PCR testing. Using a convenience sampling method, 195 were included in the study. Demographic information and some red blood cell parameters, including Hb, HCT, MCV and some LFTs such as AST, ALT, ALKP, Total bilirubin and PT, were recorded from the patient’s file. Patient outcomes were recovery or discharge from the hospital, death, and length of hospitalization. Mean±SD were used to describe quantitative variables and frequency and percentage were used to describe qualitative variables. Shapiro-Wilk test was used to check the normality of the data. Mann-Whitney U test and Spearman correlation test were used to examine the relationship between quantitative variables. The significance level was set at 0.05.
Results
In this study, the mean age of the patients was 58.92±16.39 years. Of 195 patients, 106(54.4%) were female, and 89(45.6%) were male. The demographic and clinical information of the patients is reported in Table 1.
Mortality was observed in 15.4% of cases (n=30), and recovery in 84.6% (n=165). None of the data had a normal distribution. The results of examining the relationship between the studied factors and the outcome of patients are reported in Table 2.
Conclusion
Overall, the findings of this study showed that age, total bilirubin, and PT are the risk factors associated with the outcome of COVID-19 patients. Also, low levels of Hb and HCT are associated with prolonged hospitalization. There is no significant association between liver enzyme parameters of ALT and AST and the outcome of patients with COVID-19. It is recommended that other prospective studies, if possible, be designed and implemented using a larger sample size and other laboratory parameters, paying attention to their impact on long-term complications in COVID-19 patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1401.160).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualizing, and methodology: Lida Mahfoozi; Validation and analysis: Mohammad Haghighi; Investigation and writing the original draft: Sepinood Rezaei; Review and editing, and project management: Paridokht Karimian Supervision: Lida Mahfoozi and Paridokht Karimian.
Conflicts of interest
The authors declared that there are no conflicts of interest in this article.
Acknowledgements
The authors would like to express their gratitude to the medical staff of Razi Hospital, Rasht, Iran.
References
- Lone SA, Ahmad A. COVID-19 pandemic - An African perspective. Emerging Microbes & Infections. 2020; 9(1):1300-8. [DOI:10.1080/22221751.2020.1775132] [PMID] [PMCID]
- Poon LLM. A Push for real normal: Mass screening for COVID-19. Clinical Chemistry. 2021; 68(1):4-6. [DOI:10.1093/clinchem/hvab190] [PMID] [PMCID]
- da Rosa Mesquita R, Francelino Silva Junior LC, Santos Santana FM, Farias de Oliveira T, Campos Alcântara R, Monteiro Arnozo G, et al. Clinical manifestations of COVID-19 in the general population: Systematic review. Wiener Klinische Wochenschrift. 2021; 133(7-8):377-82. [DOI:10.1007/s00508-020-01760-4] [PMID] [PMCID]
- Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, et al. Hematological findings and complications of COVID-19. American Journal of Hematology. 2020; 95(7):834-47. [DOI:10.1002/ajh.25829] [PMID] [PMCID]
- Li J, Xu G, Yu H, Peng X, Luo Y, Cao C. Clinical Characteristics and Outcomes of 74 Patients With Severe or Critical COVID-19. The American Journal of the Medical Sciences. 2020; 360(3):229-35. [DOI:10.1016/j.amjms.2020.05.040] [PMID] [PMCID]
- Li Y, Xiao SY. Hepatic involvement in COVID-19 patients: Pathology, pathogenesis, and clinical implications. Journal of Medical Virology. 2020; 92(9):1491-4. [DOI:10.1002/jmv.25973] [PMID]
- Chu H, Bai T, Chen L, Hu L, Xiao L, Yao L, et al. Multicenter Analysis of Liver Injury Patterns and Mortality in COVID-19. Frontiers in Medicine. 2020; 7:584342. [DOI:10.3389/fmed.2020.584342] [PMID] [PMCID]
- Ali MR, Hasan MA, Rahman MS, Billah M, Karmakar S, Shimu AS, et al. Clinical manifestations and socio-demographic status of COVID-19 patients during the second-wave of pandemic: A Bangladeshi experience. Journal of Infection and Public Health. 2021; 14(10):1367-1374. [DOI:10.1016/j.jiph.2021.06.011] [PMID] [PMCID]
- Schattenberg JM, Labenz C, Wörns MA, Menge P, Weinmann A, Galle PR, et al. Patterns of liver injury in COVID-19 - A German case series. United European Gastroenterology Journal. 2020; 8(7):814-9. [DOI:10.1177/2050640620931657] [PMID] [PMCID]
- Ali N, Hossain K. Liver injury in severe COVID-19 infection: Current insights and challenges. Expert Review of Gastroenterology & Hepatology. 2020; 14(10):879-84. [DOI:10.1080/17474124.2020.1794812] [PMID]
- Li S, Li J, Zhang Z, Tan L, Shao T, Li M, Li X, Holmes JA, Lin W, Han M. COVID-19 induced liver function abnormality associates with age. Aging. 2020; 12(14):13895-904. [DOI:10.18632/aging.103720] [PMID] [PMCID]
- Piano S, Dalbeni A, Vettore E, Benfaremo D, Mattioli M, Gambino CG, et al. Abnormal liver function tests predict transfer to intensive care unit and death in COVID-19. Liver International. 2020; 40(10):2394-406. [DOI:10.1111/liv.14565] [PMID] [PMCID]
- Alqahtani SA, Schattenberg JM. Liver injury in COVID-19: The current evidence. United European Gastroenterology Journal. 2020; 8(5):509-19. [DOI:10.1177/2050640620924157] [PMID] [PMCID]
- Faghani M, Naseri E, Mohammadghasemi F, Karimian P. Histopathology changes of lung, liver and heart of patients with COVID-19 in Razi hospital of Rasht. Journal of Knowledge & Health in Basic Medical Sciences. 2021; 16(3):56-65. [DOI:10.22100/jkh.v16i3.2586]
- Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clinical Chemistry and Laboratory Medicine. 2020; 58(7):1021-8. [DOI:10.1515/cclm-2020-0369] [PMID]
- Tao Z, Xu J, Chen W, Yang Z, Xu X, Liu L, et al. Anemia is associated with severe illness in COVID-19: A retrospective cohort study. Journal of Medical Virology. 2021; 93(3):1478-88. [DOI:10.1002/jmv.26444] [PMID] [PMCID]
- Algassim AA, Elghazaly AA, Alnahdi AS, Mohammed-Rahim OM, Alanazi AG, Aldhuwayhi NA, et al. Prognostic significance of hemoglobin level and autoimmune hemolytic anemia in SARS-CoV-2 infection. Annals of Hematology. 2021; 100(1):37-43. [DOI:10.1007/s00277-020-04256-3] [PMID] [PMCID]
- Taneri PE, Gómez-Ochoa SA, Llanaj E, Raguindin PF, Rojas LZ, Roa-Díaz ZM, et al. Anemia and iron metabolism in COVID-19: A systematic review and meta-analysis. European Journal of Epidemiology. 2020; 35(8):763-73. [DOI:10.1007/s10654-020-00678-5] [PMID] [PMCID]
- Chaibi S, Boussier J, Hajj WE, Abitbol Y, Taieb S, Horaist C, et al. Liver function test abnormalities are associated with a poorer prognosis in Covid-19 patients: Results of a French cohort. Clinics and Research in Hepatology and Gastroenterology. 2021; 45(5):101556. [DOI:10.1016/j.clinre.2020.10.002] [PMID] [PMCID]
- Liu Z, Li J, Long W, Zeng W, Gao R, Zeng G, et al. Bilirubin levels as potential indicators of disease severity in coronavirus disease patients: A retrospective cohort study. Frontiers in Medicine. 2020; 7:598870. [DOI:10.3389/fmed.2020.598870] [PMID] [PMCID]
- Baranovskii DS, Klabukov ID, Krasilnikova OA, Nikogosov DA, Polekhina NV, Baranovskaia DR, et al. Prolonged prothrombin time as an early prognostic indicator of severe acute respiratory distress syndrome in patients with COVID-19 related pneumonia. Current Medical Research and Opinion. 2021; 37(1):21-5. [DOI:10.1080/03007995.2020.1853510] [PMID] [PMCID]
- Long H, Nie L, Xiang X, Li H, Zhang X, Fu X, et al. D-dimer and prothrombin time are the significant indicators of severe COVID-19 and poor prognosis. BioMed Research International. 2020; 2020:6159720. [DOI:10.1155/2020/6159720] [PMID] [PMCID]
- Wang L, He WB, Yu XM, Hu DL, Jiang H. Prolonged prothrombin time at admission predicts poor clinical outcome in COVID-19 patients. World J Clin Cases. 2020; 8(19):4370-9. [DOI:10.12998/wjcc.v8.i19.4370] [PMID] [PMCID]
- Jin S, Jin Y, Xu B, Hong J, Yang X. Prevalence and impact of coagulation dysfunction in COVID-19 in China: A meta-analysis. Thrombosis and Haemostasis. 2020; 120(11):1524-35. [DOI:10.1055/s-0040-1714369] [PMID] [PMCID]
- Russo A, Tellone E, Barreca D, Ficarra S, Laganà G. Implication of COVID-19 on erythrocytes functionality: Red blood cell biochemical implications and morpho-functional aspects. International Journal of Molecular Sciences. 2022; 23(4):2171. [DOI:10.3390/ijms23042171] [PMID] [PMCID]
- Jalil AT, Shanshool MT, Dilfy SH, Saleh MM, Suleiman AA. Hematological and serological parameters for detection of COVID-19. Journal of Microbiology, Biotechnology and Food Sciences. 2022; 11(4):1-4. [DOI:10.55251/jmbfs.4229]
- Faghih Dinevari M, Somi MH, Sadeghi Majd E, Abbasalizad Farhangi M, Nikniaz Z. Anemia predicts poor outcomes of COVID-19 in hospitalized patients: A prospective study in Iran. BMC Infectious Diseases. 2021; 21(1):170. [DOI:10.1186/s12879-021-05868-4] [PMID] [PMCID]
- Tremblay D, Rapp JL, Alpert N, Lieberman-Cribbin W, Mascarenhas J, Taioli E, et al. Mild anemia as a single independent predictor of mortality in patients with COVID-19. EJHaem. 2021; 2(3):319-326. [DOI:10.1002/jha2.167] [PMID] [PMCID]
- Bloom PP, Pasricha TS, Andersson KL, Pratt DS, Hashemi N, Bhan I, et al. Hepatology consultants often disagree on etiology of abnormal liver biochemistries in COVID-19 but agree on management. Digestive Diseases and Sciences. 2021; 66(6):1852-4. [DOI:10.1007/s10620-020-06495-w] [PMID] [PMCID]
- Saini RK, Saini N, Ram S, Soni SL, Suri V, Malhotra P, et al. COVID-19 associated variations in liver function parameters: a retrospective study. Postgraduate Medical Journal. 2022; 98(1156):91-7. [DOI:10.1136/postgradmedj-2020-138930] [PMID]
Review Paper: Research |
Subject:
General
Received: 2023/05/17 | Accepted: 2024/10/6 | Published: 2025/04/1
Received: 2023/05/17 | Accepted: 2024/10/6 | Published: 2025/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |