Volume 34, Issue 3 (10-2025)
JGUMS 2025, 34(3): 294-307 |
Back to browse issues page
Research code: 613
Ethics code: IR.GUMS.REC.1398.300
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azizzade Dobakhshari M, Samidoust P, Razaghi K, Badsar E, Badsar A. The General Surgery Malpractice Rate and the Related Factors in Guilan Province, North of Iran, From 2011 to 2017. JGUMS 2025; 34 (3) :294-307
URL: http://journal.gums.ac.ir/article-1-2728-en.html
URL: http://journal.gums.ac.ir/article-1-2728-en.html
Mahan Azizzade Dobakhshari1 

 , Pirouz Samidoust2
, Pirouz Samidoust2 

 , Kiavash Razaghi3
, Kiavash Razaghi3 

 , Erfan Badsar3
, Erfan Badsar3 

 , Alireza Badsar *4
, Alireza Badsar *4 




 , Pirouz Samidoust2
, Pirouz Samidoust2 

 , Kiavash Razaghi3
, Kiavash Razaghi3 

 , Erfan Badsar3
, Erfan Badsar3 

 , Alireza Badsar *4
, Alireza Badsar *4 


1- Urology Research Center, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Surgery, Medical Education Research Center, Faculty of Medicine, Razi Hospital, Gilan University of Medical Sciences, Rasht, Iran.
3- Razi Clinical Research Development Unit, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Forensic Medicine, Social Determinants of Health Research Center, Faculty of Medicine, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Surgery, Medical Education Research Center, Faculty of Medicine, Razi Hospital, Gilan University of Medical Sciences, Rasht, Iran.
3- Razi Clinical Research Development Unit, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Forensic Medicine, Social Determinants of Health Research Center, Faculty of Medicine, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 4073 kb]
(176 Downloads)
| Abstract (HTML) (854 Views)
Full-Text: (306 Views)
Introduction
Medical malpractice refers to treatments that do not meet accepted medical standards and result in harm, disability, or death. Furthermore, malpractice is a relative concept, and knowledge levels vary among doctors. In addition to causing public health concerns, malpractice affects physicians’ personal and professional lives. When a doctor fails in diagnosis, treatment, or follow-up, resulting in patient harm, s/he has committed medical malpractice. However, not all treatment failures are due to malpractice, as medicine involves uncertainty, and even skilled doctors may experience unsuccessful outcomes. One major consequence is the formation of defensive medicine, where doctors, fearing lawsuits, order unnecessary tests or avoid high-risk treatments, which can compromise care quality and trust in the doctor-patient relationship. Although medical malpractice cases represent a small part of adverse healthcare system outcomes, they remain a valuable indicator of healthcare system quality.
Despite medical advancements, medical malpractice claims are increasing globally, including in Iran, leading to decreased public trust and increased stress among both patients and physicians. These claims also impose emotional and financial burdens on the affected people. Given the cultural and systemic differences in how medical malpractice is handled, local studies—especially in high-risk fields such as general surgery—are crucial for identifying causes, improving safety, and restoring public confidence. The present study aims to investigate the frequency of medical malpractice in the field of general surgery and the associated factors in Guilan Province, north of Iran, from 2011 to 2017.
Methods
This descriptive retrospective study reviewed medical malpractice complaints in general surgery sent to the Legal Medicine Organization of Guilan Province from 2011 to 2017. After obtaining ethical approval and necessary permissions, the cases were analyzed, and the data, including patients’ demographic information, type of treatment, surgical details, cause of malpractice, and the verdict of the Medical Commission, were extracted using a checklist. Data were entered into SPSS software, version 21 and analyzed using descriptive statistics, the chi-square test, and Fisher’s exact test, considering a significance level set at 0.05.
Results
This study examined 84 medical malpractice complaint cases related to general surgery. Of these cases, 48 were related to male patients and 36 to female patients. As shown in Table 1, in 43 cases (51.19%), the verdict was rendered against the physician, while in 41 cases (48.81%), the physician was acquitted. Notably, none of the cases ended due to patient satisfaction or reconciliation between the parties. Regarding the type of medical center, 41 patients (48.81%) had general surgery at public teaching centers, 6 (7.14%) at public non-teaching centers, and 37 (44.05%) at private centers. In 57 cases, the complaints were related to elective treatments, while 27 cases (32.14%) were related to emergency treatments. The abdomen was the most commonly affected organ by malpractice (n=46, 54.76%), followed by the upper limbs (n=18, 21.43%).
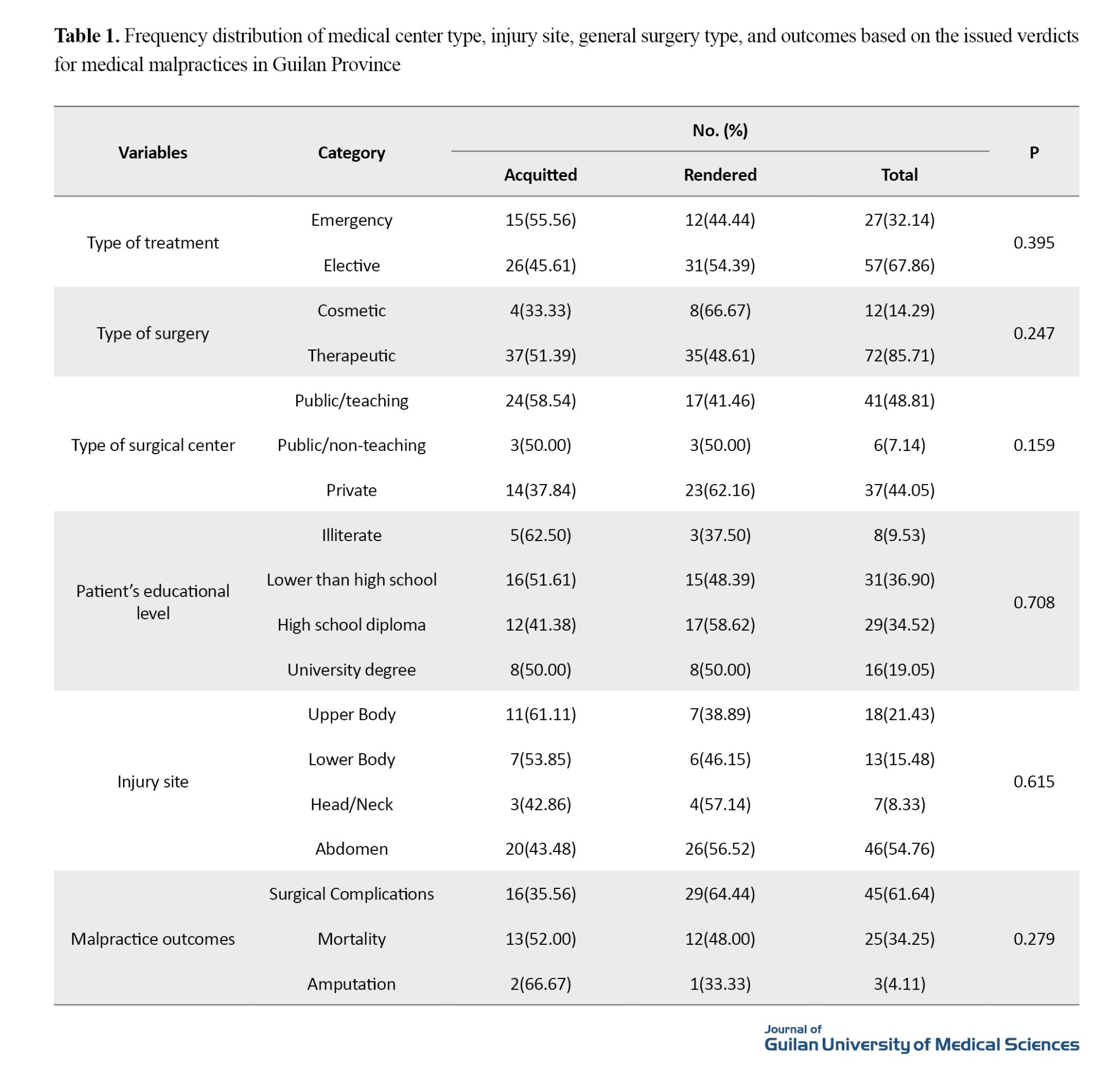
We found no statistically significant difference in the malpractice rate between male (47.92%) and female (55.56%) patients (P= 0.097). Similarly, no significant differences were found based on patients’ age (P=0.097), gender (P=0.488), or marital status (P=0.355). The malpractice rate was not significantly different based on the type of medical center, the injured site, or the nature of harm caused by malpractice, either.
Although malpractice rates were higher in elective treatments compared to emergency treatments, as well as in cosmetic surgeries compared to therapeutic surgeries, these differences were not statistically significant (P>0.05). Surgical complications were more common than amputations or deaths (as outcomes of malpractice), but the difference was not statistically significant.
The physicians who were not general surgeons and those with board certification had higher malpractice rates compared to board-certified general surgeons. However, this difference was also not statistically significant.
Conclusion
In about 51% of complaints in Guilan Province regarding general surgery malpractice, the verdict was rendered against the physicians. The current study found 16.67% of malpractice cases were due to negligence and 28.57% due to a combination of factors such as lack of skills, carelessness, negligence, and failure to comply with government regulations. There is a need for more comprehensive studies to explore potential risk factors and improve patient safety in surgical practices.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.300). To maintain confidentiality, the review of cases was done onsite, and complainants’ personal information was not recorded.
Funding
This research did not receive any financial support from funding organizations in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Alireza Badsar, Mahan Azizzade Dobakhshari; data collection: Alireza Badsar, Mahan Azizzade Dobakhshari, Pirooz Samidoust, and Kiavash Razaghi; validation: Alireza Badsar, Pirooz Samidoust, and Erfan Badsar; data analysis and investigation: Mahan Azizzade Dobakhshari, Pirooz Samidoust, and Erfan Badsar; resources: Kiavash Razaghi, Alireza Badsar, and Erfan Badsar; initial draft preparation: Mahan Azizzade Dobakhshari, Kiavash Razaghi, and Alireza Badsar; editing & review: Mahan Azizzade Dobakhshari, Pirooz Samidoust, and Alireza Badsar; supervision, project management; validation: Mahan Azizzade Dobakhshari and Erfan Badsar.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
The authors would like to thank the Department of Forensic Medicine at Guilan University of Medical Sciences, and Mr. Mehdi Ghorbani Samim (the former head of the Guilan Legal Medicine Organization) for their support and assistance in this research.
Medical malpractice refers to treatments that do not meet accepted medical standards and result in harm, disability, or death. Furthermore, malpractice is a relative concept, and knowledge levels vary among doctors. In addition to causing public health concerns, malpractice affects physicians’ personal and professional lives. When a doctor fails in diagnosis, treatment, or follow-up, resulting in patient harm, s/he has committed medical malpractice. However, not all treatment failures are due to malpractice, as medicine involves uncertainty, and even skilled doctors may experience unsuccessful outcomes. One major consequence is the formation of defensive medicine, where doctors, fearing lawsuits, order unnecessary tests or avoid high-risk treatments, which can compromise care quality and trust in the doctor-patient relationship. Although medical malpractice cases represent a small part of adverse healthcare system outcomes, they remain a valuable indicator of healthcare system quality.
Despite medical advancements, medical malpractice claims are increasing globally, including in Iran, leading to decreased public trust and increased stress among both patients and physicians. These claims also impose emotional and financial burdens on the affected people. Given the cultural and systemic differences in how medical malpractice is handled, local studies—especially in high-risk fields such as general surgery—are crucial for identifying causes, improving safety, and restoring public confidence. The present study aims to investigate the frequency of medical malpractice in the field of general surgery and the associated factors in Guilan Province, north of Iran, from 2011 to 2017.
Methods
This descriptive retrospective study reviewed medical malpractice complaints in general surgery sent to the Legal Medicine Organization of Guilan Province from 2011 to 2017. After obtaining ethical approval and necessary permissions, the cases were analyzed, and the data, including patients’ demographic information, type of treatment, surgical details, cause of malpractice, and the verdict of the Medical Commission, were extracted using a checklist. Data were entered into SPSS software, version 21 and analyzed using descriptive statistics, the chi-square test, and Fisher’s exact test, considering a significance level set at 0.05.
Results
This study examined 84 medical malpractice complaint cases related to general surgery. Of these cases, 48 were related to male patients and 36 to female patients. As shown in Table 1, in 43 cases (51.19%), the verdict was rendered against the physician, while in 41 cases (48.81%), the physician was acquitted. Notably, none of the cases ended due to patient satisfaction or reconciliation between the parties. Regarding the type of medical center, 41 patients (48.81%) had general surgery at public teaching centers, 6 (7.14%) at public non-teaching centers, and 37 (44.05%) at private centers. In 57 cases, the complaints were related to elective treatments, while 27 cases (32.14%) were related to emergency treatments. The abdomen was the most commonly affected organ by malpractice (n=46, 54.76%), followed by the upper limbs (n=18, 21.43%).
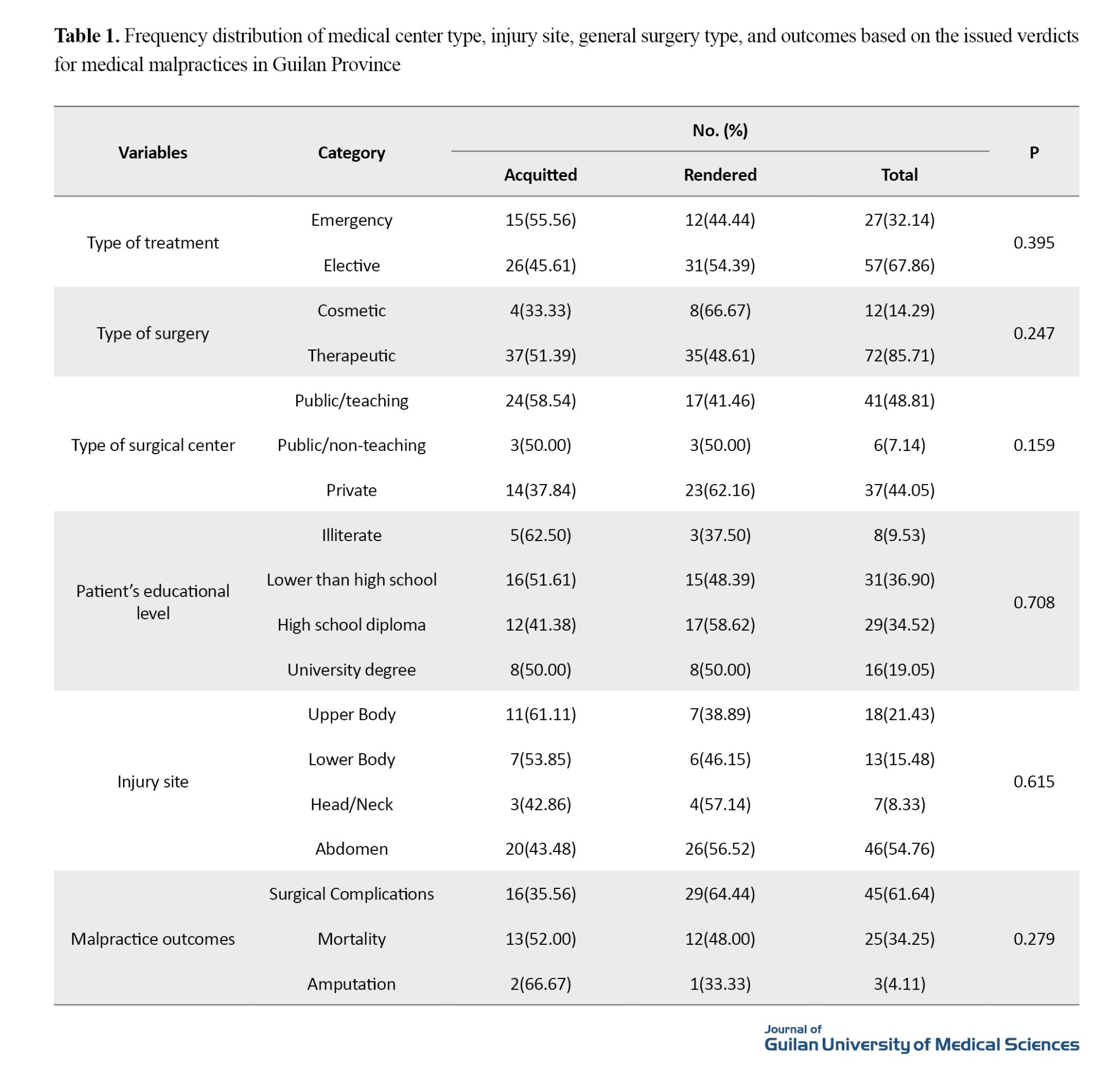
We found no statistically significant difference in the malpractice rate between male (47.92%) and female (55.56%) patients (P= 0.097). Similarly, no significant differences were found based on patients’ age (P=0.097), gender (P=0.488), or marital status (P=0.355). The malpractice rate was not significantly different based on the type of medical center, the injured site, or the nature of harm caused by malpractice, either.
Although malpractice rates were higher in elective treatments compared to emergency treatments, as well as in cosmetic surgeries compared to therapeutic surgeries, these differences were not statistically significant (P>0.05). Surgical complications were more common than amputations or deaths (as outcomes of malpractice), but the difference was not statistically significant.
The physicians who were not general surgeons and those with board certification had higher malpractice rates compared to board-certified general surgeons. However, this difference was also not statistically significant.
Conclusion
In about 51% of complaints in Guilan Province regarding general surgery malpractice, the verdict was rendered against the physicians. The current study found 16.67% of malpractice cases were due to negligence and 28.57% due to a combination of factors such as lack of skills, carelessness, negligence, and failure to comply with government regulations. There is a need for more comprehensive studies to explore potential risk factors and improve patient safety in surgical practices.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.300). To maintain confidentiality, the review of cases was done onsite, and complainants’ personal information was not recorded.
Funding
This research did not receive any financial support from funding organizations in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Alireza Badsar, Mahan Azizzade Dobakhshari; data collection: Alireza Badsar, Mahan Azizzade Dobakhshari, Pirooz Samidoust, and Kiavash Razaghi; validation: Alireza Badsar, Pirooz Samidoust, and Erfan Badsar; data analysis and investigation: Mahan Azizzade Dobakhshari, Pirooz Samidoust, and Erfan Badsar; resources: Kiavash Razaghi, Alireza Badsar, and Erfan Badsar; initial draft preparation: Mahan Azizzade Dobakhshari, Kiavash Razaghi, and Alireza Badsar; editing & review: Mahan Azizzade Dobakhshari, Pirooz Samidoust, and Alireza Badsar; supervision, project management; validation: Mahan Azizzade Dobakhshari and Erfan Badsar.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
The authors would like to thank the Department of Forensic Medicine at Guilan University of Medical Sciences, and Mr. Mehdi Ghorbani Samim (the former head of the Guilan Legal Medicine Organization) for their support and assistance in this research.
References
- Sloan FA., Hsieh CR. Health economics. Cambridge: The MIT Press; 2017. [Link]
- Akachi Y, Tarp F, Kelley E, Addisona T, Kruk ME. Measuring quality-of-care in the context of sustainable development goal 3: A call for papers. Bulletin of the World Health Organization. 2016; 94(3):160-160A. [DOI:10.2471/BLT.16.170605] [PMID] [PMCID]
- AdibZadeh A, Ghadi Pasha M, Pour Amiri A, Nakhaei N, Samadi Rad B, Bastani M. [A study on medical malpractices ending to death and disability referred to Kerman Medical council’s medical malpractices commission (Persian)]. Medical Law Journal. 2012; 6(20):141-54. [Link]
- Mechanic, D., Some social aspects of the medical malpractice dilemma. Duke Law Journal. 1975; 1975(6):1179. [DOI:10.2307/1372062]
- Monaghan L, Gabe J. Key concepts in medical sociology. Los Angeles: Sage; 2013. [DOI:10.4135/9781526401687]
- Järvelin J, Häkkinen U. Can patient injury claims be utilised as a quality indicator? Health Policy. 2012; 104(2):155-62. [DOI:10.1016/j.healthpol.2011.08.012] [PMID]
- Siabani S, Alipour AA, Siabani H, Rezaei M, Daniali S. A survey of complaints against physicians reviewed at Kermanshah. Journal of Kermanshah University of Medical Sciences. 2009. 13(1):e79831. [Link]
- Yoo JH, Chang CB, Kang YG, Kim SJ, Seong SC, Kim TK. Patient expectations of total knee replacement and their association with sociodemographic factors and functional status. The Journal of Bone and Joint Surgery. British volume. 2011; 93(3):337-44. [DOI:10.1302/0301-620X.93B3.25168] [PMID]
- Aghakhani N, Cheraghi R, Zarei A, Alinejad V. Study of causes of health providers' malpractices in records referred to Forensic Medicine Organization in Urmia, during 2009-2013. The Iranian Journal of Medical Law. 2017; 11(42):83-100. [Link]
- Pandit MS, Pandit S. Medical negligence: Criminal prosecution of medical professionals, importance of medical evidence: Some guidelines for medical practitioners. Indian Journal of Urology. 2009; 25(3):379-83. [DOI:10.4103/0970-1591.56207] [PMID] [PMCID]
- Shahabedin Sadr S, Ghadyani MH, Avish S, Ramim T. Medical malpractice frequency in the psychiatric field, in Medical Council of Iran, from 2001 to 2010: A brief report. Tehran University Medical Journal. 2014; 72(5):329. [Link]
- Bagherian Mahmoodabadi H, Setareh M, Nejadnick M, Niknamian M, Aubian A. [The frequency and reasons of medical errors in cases referred to Isfahan legal medicine center (Persian)]. Health Information Management. 2012; 9(1):101-9. [Link]
- Bernstein M, Hebert PC, Etchells E. Patient safety in neurosurgery: Detection of errors, prevention of errors, and disclosure of errors. Neurosurgery Quarterly. 2003; 13(2):125-37. [DOI:10.1097/00013414-200306000-00008]
- Balch CM, Oreskovich MR, Dyrbye LN, Colaiano JM, Satele DV, Sloan JA, et al. Personal consequences of malpractice lawsuits on American surgeons. Journal of the American College of Surgeons. 2011; 213(5):657-67. [DOI:10.1016/j.jamcollsurg.2011.08.005] [PMID]
- Wang Z, Li N, Jiang M, Dear K, Hsieh CR. Records of medical malpractice litigation: A potential indicator of health-care quality in China. Bulletin of the World Health Organization. 2017; 95(6):430-6. [DOI:10.2471/BLT.16.179143] [PMID] [PMCID]
- Şen H, Aliustaoğlu S, Sezer Y, İnce CH. Evaluation of the medical malpractice cases concluded in the general assembly of council of forensic medicine. Turkish Journal of Trauma and Emergency Surgery. 2015; 21(3):204-8. [DOI:10.5505/tjtes.2015.24295]
- Moghimi N, Sabzevari S, Nasiri Kalmarzi R, Shafei A, Yousefinejad V. Frequency of medical malpractice in deceased patients' records in Tohid Hospital in Sanandaj in 2017. Scientific Journal of Kurdistan University of Medical Sciences. 2019; 24(1):90-7. [Link]
Review Paper: Research |
Subject:
General
Received: 2024/09/24 | Accepted: 2025/02/18 | Published: 2025/10/2
Received: 2024/09/24 | Accepted: 2025/02/18 | Published: 2025/10/2
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |