Volume 34, Issue 2 (7-2025)
JGUMS 2025, 34(2): 192-209 |
Back to browse issues page
Research code: 000
Ethics code: IR.GUMS.REC.1398.459
Clinical trials code: 0
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zohrevandi B, Azizzade Dobakhshari M, Zia Ziabari S M, Kazemnejhad-Leili E, Saberi J, Rimaz S. Evaluating Serum Lactate and Base Deficit as Predictive Tools for Mortality in Patients With Burns of 20% or Greater. JGUMS 2025; 34 (2) :192-209
URL: http://journal.gums.ac.ir/article-1-2731-en.html
URL: http://journal.gums.ac.ir/article-1-2731-en.html
Behzad Zohrevandi1 
 , Mahan Azizzade Dobakhshari2
, Mahan Azizzade Dobakhshari2 
 , Seyyed Mahdi Zia Ziabari3
, Seyyed Mahdi Zia Ziabari3 
 , Ehsan Kazemnejhad-Leili2
, Ehsan Kazemnejhad-Leili2 
 , Jafar Saberi4
, Jafar Saberi4 
 , Siamak Rimaz *5
, Siamak Rimaz *5 


 , Mahan Azizzade Dobakhshari2
, Mahan Azizzade Dobakhshari2 
 , Seyyed Mahdi Zia Ziabari3
, Seyyed Mahdi Zia Ziabari3 
 , Ehsan Kazemnejhad-Leili2
, Ehsan Kazemnejhad-Leili2 
 , Jafar Saberi4
, Jafar Saberi4 
 , Siamak Rimaz *5
, Siamak Rimaz *5 

1- Department of Emergency Medicine, Road Trauma Research Center, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Urology Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Emergency Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Clinical Research Development, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Anesthesiology, Anesthesia Research Center, School of Medicine, Al-Zahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Urology Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Emergency Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Clinical Research Development, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Anesthesiology, Anesthesia Research Center, School of Medicine, Al-Zahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 6689 kb]
(247 Downloads)
| Abstract (HTML) (947 Views)
Full-Text: (410 Views)
Introduction
Severe burns cause microvascular damage, leading to rapid fluid loss, hypovolemic shock and reduced organ perfusion. A 2023 study on 2651 burn patients in Spain found that most were male (61%), with scalding as the leading cause. Mortality (4.3%) was linked to age, smoke inhalation, and full-thickness burns, with multiorgan failure being the primary cause of death. Fluid resuscitation (2–4mL×%TBSA×kg total body surface area [TBSA] in 24 h) is critical but controversial, as over-resuscitation worsens edema and hypoperfusion. Ideal markers, like serum lactate and base deficit, help detect hypoxia and guide therapy, though optimal endpoints remain debated. Traditional monitoring (urine output, blood pressure) may delay shock detection, increasing infection and mortality risks. Invasive tools (e.g. central venous pressure) improve precision but are costly and risky. Global oxygenation indices (e.g. gastric pH) are more predictive than practical. Ultimately, organ perfusion is the resuscitation goal, with lactate reflecting oxygen imbalance and prognosis. This study evaluates whether serum lactate and base deficit can predict mortality in burn patients, addressing gaps in current monitoring and resuscitation strategies.
Methods
This cross-sectional study analyzed 389 burn patients (≥20% TBSA) admitted to Velayat Hospital, Iran (March-September 2019) to evaluate resuscitation outcomes. The cohort comprised conscious adults (>18 years), with consent obtained from relatives for unconscious patients, while excluding those with pre-existing cardiopulmonary conditions, inhalation injuries, or early mortality (<48 h). Burn severity was assessed using Liu’s method, with fluid resuscitation guided by the Parkland formula (4 mL/kg/% TBSA of Lactated Ringer’s), titrated to maintain urine output at 1 mL/kg/h and mean arterial pressure ≥ 65 mmHg. Intensive monitoring included q2 h vital signs and urine output measurements, plus serial arterial blood sampling (q12 h for 48 h) to analyze serum lactate (normal ≤2 mmol/L) and base deficit using standardized HITACHI/ROCHEH analyzers, with single-laboratory protocols minimizing variability. Comprehensive data collection captured demographics, burn characteristics, resuscitation parameters and clinical outcomes, with separate analysis for inhalation injury subgroups. Statistical processing using the SPSS software, version 21, employed descriptive analyses, independent t-tests, chi-square tests and multivariate regression (COX repeated measure analysis of variance), with significance set at P<0.05. The study design emphasized rigorous biomarker monitoring to assess their predictive value for mortality and organ failure while maintaining methodological consistency through centralized laboratory analysis and blinded outcome assessment where applicable.
Results
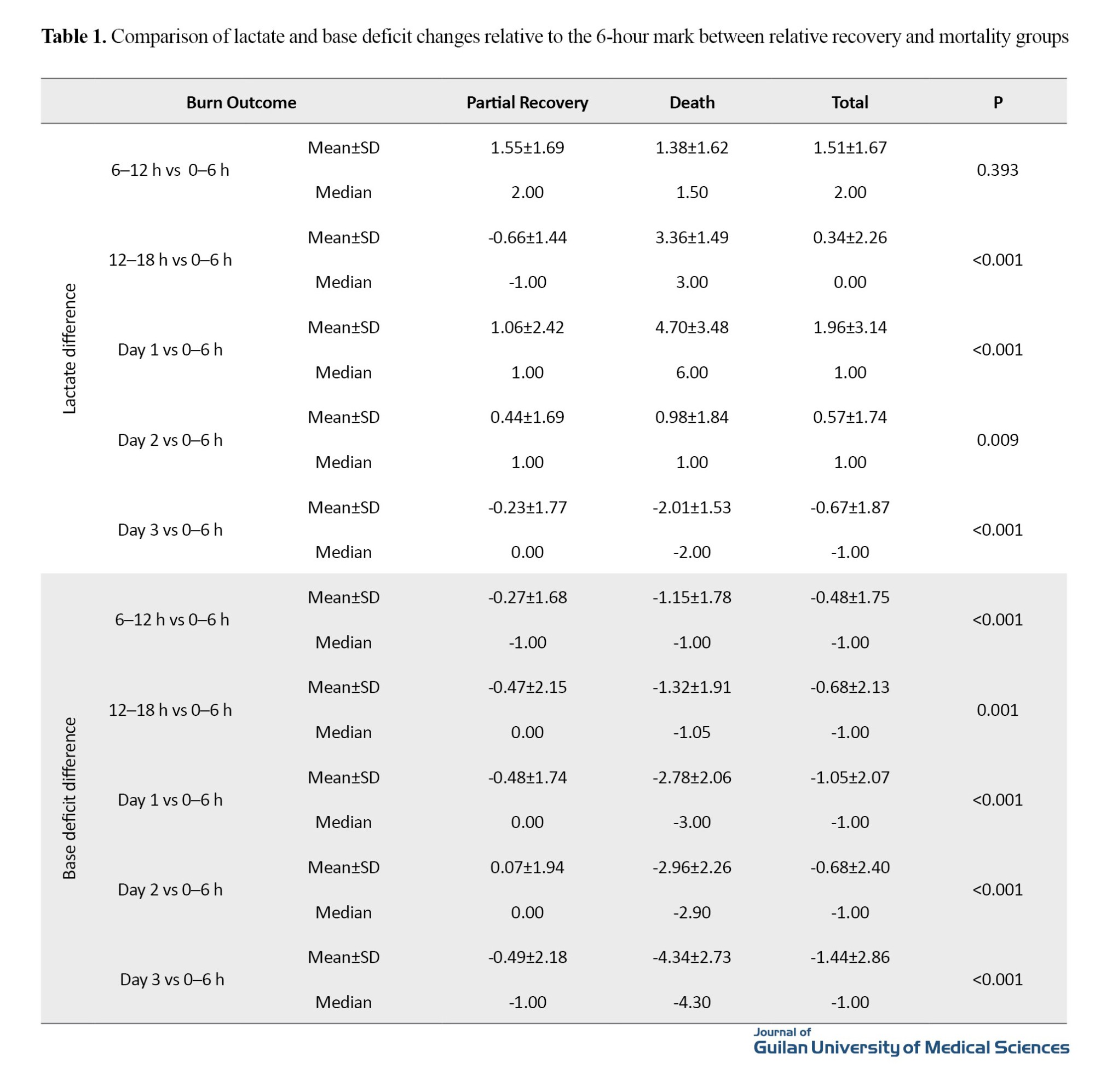
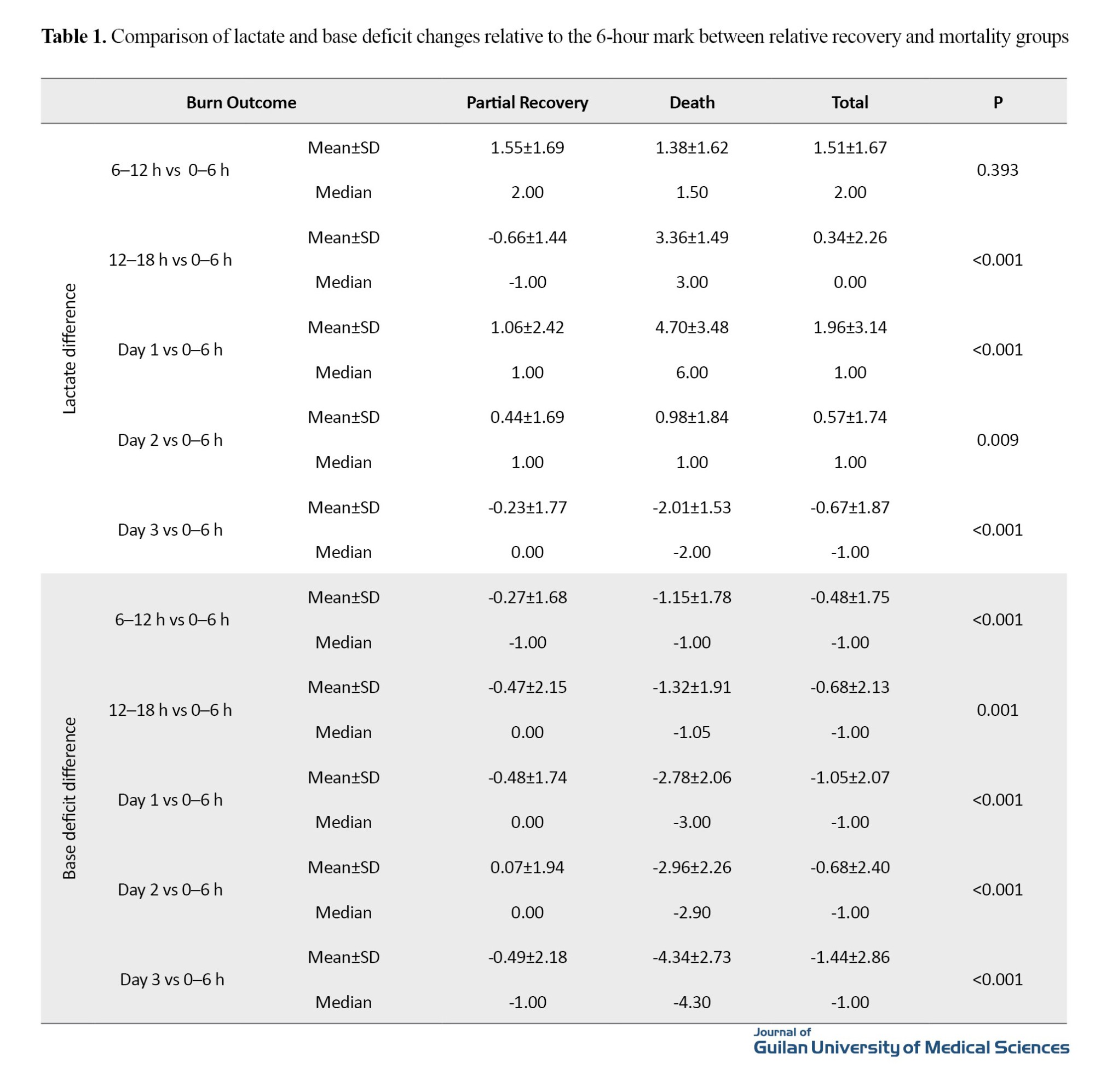
This study analyzed 389 severe burn patients (≥20% TBSA) admitted to Velayat Burn Center in Rasht City, Iran, to evaluate the predictive value of serum lactate and base deficit for mortality outcomes. The cohort had a mean age of 31.8±41.9 years (range 19-92 years), was predominantly male (77.6%), and presented with a mean burn extent of 43.1±23.3% TBSA, mostly third-degree burns (62.9%). Key findings revealed a 24.7% mortality rate, significantly associated with older age (≥35 years), larger burn extent (50-75% TBSA: 59.2% mortality; >75%: 88.9%) and higher burn degree (fourth-degree: 78.1% mortality). Serial biomarker measurements demonstrated that non-survivors maintained significantly higher lactate levels (P<0.001) throughout hospitalization, peaking at 6-24 h post-injury before declining, while survivors showed consistent reduction (P<0.001). Base deficit similarly distinguished outcomes at all timepoints (P<0.001). Receiver operating characteristic analysis identified optimal predictive windows: lactate at 18 h post-admission showed the strongest predictive value (area under curve [AUC]=0.997), with cutoff of 4.5 mmol/L (96.9% sensitivity, 95.9% specificity), while base deficit at 6 hours post-admission was most predictive (AUC=0.964) at -3.25 cutoff (94.5% sensitivity, 96.9% specificity). Multivariate analysis confirmed both biomarkers as independent mortality predictors after controlling for sex, burn characteristics and sampling time (P<0.001), with a particularly strong association for lactate (partial Eta squared=0.863). The results demonstrate that early (6-18 h) serial measurements of lactate and base deficit provide robust, time-sensitive mortality prediction in severe burns, maintaining prognostic value even after adjusting for confounding factors.
These findings support incorporating these readily available biomarkers into standard burn resuscitation protocols to improve risk stratification, with lactate levels >4.5 mmol/L at 18 h and base deficit <-3.25 at 6 h serving as critical thresholds for identifying high-risk patients. The study highlights the importance of dynamic biomarker monitoring rather than single measurements, as the temporal patterns (particularly the 6-24 h lactate surge in non-survivors) provide crucial prognostic information beyond absolute values. These results have immediate clinical applicability for burn centers, suggesting that early identification of high-risk patients through this monitoring approach could guide more aggressive interventions and resource allocation, potentially improving outcomes in this vulnerable population. The strong predictive performance maintained after multivariate adjustment reinforces the utility of these biomarkers across diverse burn patient demographics and injury patterns (Table 1).
Conclusion
This study analyzed 389 severe burn patients (≥20% TBSA), finding 25% mortality. Key predictors included age≥35 years (higher mortality), larger burns (50-75% TBSA: 59.2%; >75%: 88.9%), and third-degree burns. Serial measurements showed non-survivors had persistently elevated lactate (peaking at 6 h) and progressively worsening base deficit. Optimal predictive thresholds were: Lactate >4.5 mmol/L at 18 h (96.9% sensitivity) and base deficit <-3.25 at 6 h (94.5% sensitivity). The study confirms these biomarkers’ value for mortality prediction, with delayed lactate clearance indicating poor prognosis. The results support incorporating serial lactate/base deficit monitoring into burn resuscitation protocols to guide treatment and improve outcomes. Limitations include a single-center retrospective design. This study confirms plasma base deficit and serum lactate as rapid, valuable markers for monitoring burn resuscitation. We established time-specific cutoff values correlating with mortality risk, enabling clinical triage of burn patients. These practical biomarkers enhance resuscitation assessment and outcome prediction in burn care, supporting their integration with standard clinical evaluation protocols.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.459. Following the guidelines of the Guilan University of Medical Sciences Ethics Committee, patient identities were kept confidential during data collection.
Funding
This research did not receive any financial support from funding organizations in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, methodology, preparing the initial draft: Behzad Zohrevandi, Siamak Rimaz, Mahan Azizzade Dobakhshari and Jafar Saberi; Validation, project management: Behzad Zohrevandi, Siamak Rimaz, Seyyed Mahdi Zia Ziabari; Data analysis and visualization: Behzad Zohrevandi, Mahan Azizzade Dobakhshari, Ehsan Kazemnezhad Leili and Jafar Saberi; Investigation and resources: Behzad Zohrevandi, Mahan Azizzade Dobakhshari and Jafar Saberi; editing & review: Siamak Rimaz, Behzad Zohrevandi and Mahan Azizzadeh Dobakhshari.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Clinical Research Development Unit of Poursina Hospital and the Velayat Burn and Regenerative Medicine Research Center in Guilan Province, and all participants for their valuable support and collaboration in this research.
Severe burns cause microvascular damage, leading to rapid fluid loss, hypovolemic shock and reduced organ perfusion. A 2023 study on 2651 burn patients in Spain found that most were male (61%), with scalding as the leading cause. Mortality (4.3%) was linked to age, smoke inhalation, and full-thickness burns, with multiorgan failure being the primary cause of death. Fluid resuscitation (2–4mL×%TBSA×kg total body surface area [TBSA] in 24 h) is critical but controversial, as over-resuscitation worsens edema and hypoperfusion. Ideal markers, like serum lactate and base deficit, help detect hypoxia and guide therapy, though optimal endpoints remain debated. Traditional monitoring (urine output, blood pressure) may delay shock detection, increasing infection and mortality risks. Invasive tools (e.g. central venous pressure) improve precision but are costly and risky. Global oxygenation indices (e.g. gastric pH) are more predictive than practical. Ultimately, organ perfusion is the resuscitation goal, with lactate reflecting oxygen imbalance and prognosis. This study evaluates whether serum lactate and base deficit can predict mortality in burn patients, addressing gaps in current monitoring and resuscitation strategies.
Methods
This cross-sectional study analyzed 389 burn patients (≥20% TBSA) admitted to Velayat Hospital, Iran (March-September 2019) to evaluate resuscitation outcomes. The cohort comprised conscious adults (>18 years), with consent obtained from relatives for unconscious patients, while excluding those with pre-existing cardiopulmonary conditions, inhalation injuries, or early mortality (<48 h). Burn severity was assessed using Liu’s method, with fluid resuscitation guided by the Parkland formula (4 mL/kg/% TBSA of Lactated Ringer’s), titrated to maintain urine output at 1 mL/kg/h and mean arterial pressure ≥ 65 mmHg. Intensive monitoring included q2 h vital signs and urine output measurements, plus serial arterial blood sampling (q12 h for 48 h) to analyze serum lactate (normal ≤2 mmol/L) and base deficit using standardized HITACHI/ROCHEH analyzers, with single-laboratory protocols minimizing variability. Comprehensive data collection captured demographics, burn characteristics, resuscitation parameters and clinical outcomes, with separate analysis for inhalation injury subgroups. Statistical processing using the SPSS software, version 21, employed descriptive analyses, independent t-tests, chi-square tests and multivariate regression (COX repeated measure analysis of variance), with significance set at P<0.05. The study design emphasized rigorous biomarker monitoring to assess their predictive value for mortality and organ failure while maintaining methodological consistency through centralized laboratory analysis and blinded outcome assessment where applicable.
Results
This study analyzed 389 severe burn patients (≥20% TBSA) admitted to Velayat Burn Center in Rasht City, Iran, to evaluate the predictive value of serum lactate and base deficit for mortality outcomes. The cohort had a mean age of 31.8±41.9 years (range 19-92 years), was predominantly male (77.6%), and presented with a mean burn extent of 43.1±23.3% TBSA, mostly third-degree burns (62.9%). Key findings revealed a 24.7% mortality rate, significantly associated with older age (≥35 years), larger burn extent (50-75% TBSA: 59.2% mortality; >75%: 88.9%) and higher burn degree (fourth-degree: 78.1% mortality). Serial biomarker measurements demonstrated that non-survivors maintained significantly higher lactate levels (P<0.001) throughout hospitalization, peaking at 6-24 h post-injury before declining, while survivors showed consistent reduction (P<0.001). Base deficit similarly distinguished outcomes at all timepoints (P<0.001). Receiver operating characteristic analysis identified optimal predictive windows: lactate at 18 h post-admission showed the strongest predictive value (area under curve [AUC]=0.997), with cutoff of 4.5 mmol/L (96.9% sensitivity, 95.9% specificity), while base deficit at 6 hours post-admission was most predictive (AUC=0.964) at -3.25 cutoff (94.5% sensitivity, 96.9% specificity). Multivariate analysis confirmed both biomarkers as independent mortality predictors after controlling for sex, burn characteristics and sampling time (P<0.001), with a particularly strong association for lactate (partial Eta squared=0.863). The results demonstrate that early (6-18 h) serial measurements of lactate and base deficit provide robust, time-sensitive mortality prediction in severe burns, maintaining prognostic value even after adjusting for confounding factors.
These findings support incorporating these readily available biomarkers into standard burn resuscitation protocols to improve risk stratification, with lactate levels >4.5 mmol/L at 18 h and base deficit <-3.25 at 6 h serving as critical thresholds for identifying high-risk patients. The study highlights the importance of dynamic biomarker monitoring rather than single measurements, as the temporal patterns (particularly the 6-24 h lactate surge in non-survivors) provide crucial prognostic information beyond absolute values. These results have immediate clinical applicability for burn centers, suggesting that early identification of high-risk patients through this monitoring approach could guide more aggressive interventions and resource allocation, potentially improving outcomes in this vulnerable population. The strong predictive performance maintained after multivariate adjustment reinforces the utility of these biomarkers across diverse burn patient demographics and injury patterns (Table 1).
Conclusion
This study analyzed 389 severe burn patients (≥20% TBSA), finding 25% mortality. Key predictors included age≥35 years (higher mortality), larger burns (50-75% TBSA: 59.2%; >75%: 88.9%), and third-degree burns. Serial measurements showed non-survivors had persistently elevated lactate (peaking at 6 h) and progressively worsening base deficit. Optimal predictive thresholds were: Lactate >4.5 mmol/L at 18 h (96.9% sensitivity) and base deficit <-3.25 at 6 h (94.5% sensitivity). The study confirms these biomarkers’ value for mortality prediction, with delayed lactate clearance indicating poor prognosis. The results support incorporating serial lactate/base deficit monitoring into burn resuscitation protocols to guide treatment and improve outcomes. Limitations include a single-center retrospective design. This study confirms plasma base deficit and serum lactate as rapid, valuable markers for monitoring burn resuscitation. We established time-specific cutoff values correlating with mortality risk, enabling clinical triage of burn patients. These practical biomarkers enhance resuscitation assessment and outcome prediction in burn care, supporting their integration with standard clinical evaluation protocols.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.459. Following the guidelines of the Guilan University of Medical Sciences Ethics Committee, patient identities were kept confidential during data collection.
Funding
This research did not receive any financial support from funding organizations in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, methodology, preparing the initial draft: Behzad Zohrevandi, Siamak Rimaz, Mahan Azizzade Dobakhshari and Jafar Saberi; Validation, project management: Behzad Zohrevandi, Siamak Rimaz, Seyyed Mahdi Zia Ziabari; Data analysis and visualization: Behzad Zohrevandi, Mahan Azizzade Dobakhshari, Ehsan Kazemnezhad Leili and Jafar Saberi; Investigation and resources: Behzad Zohrevandi, Mahan Azizzade Dobakhshari and Jafar Saberi; editing & review: Siamak Rimaz, Behzad Zohrevandi and Mahan Azizzadeh Dobakhshari.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the Clinical Research Development Unit of Poursina Hospital and the Velayat Burn and Regenerative Medicine Research Center in Guilan Province, and all participants for their valuable support and collaboration in this research.
References
- Holm C, Melcer B, Hörbrand F, Wörl H, von Donnersmarck GH, Mühlbauer W. Intrathoracic blood volume as an end point in resuscitation of the severely burned: An observational study of 24 patients. The Journal of Trauma: Injury, Infection, and Critical Care. 2000; 48(4):728-34. [DOI:10.1097/00005373-200004000-00023] [PMID]
- Germann G, Steinau HU. [Current aspects of burn treatment (German)]. Zentralblatt fur Chirurgie. 1993; 118(5):290-302. [PMID]
- Abarca L, Guilabert P, Martin N, Usúa G, Barret JP, Colomina MJ. Epidemiology and mortality in patients hospitalized for burns in Catalonia, Spain. Scientific Reports. 2023; 13(1):14364. [DOI:10.1038/s41598-023-40198-2] [PMID]
- Cartotto RC, Innes M, Musgrave MA, Gomez M, Cooper AB. How well does the Parkland formula estimate actual fluid resuscitation volumes? The Journal of Burn Care & Rehabilitation. 2002; 23(4):258-65. [DOI:10.1097/00004630-200207000-00006] [PMID]
- Saffle JR. The phenomenon of “fluid creep” in acute burn resuscitation. Journal of Burn Care & Research. 2007; 28(3):382-95. [DOI:10.1097/BCR.0B013E318053D3A1] [PMID]
- Kamolz LP, Andel H, Schramm W, Meissl G, Herndon DN, Frey M. Lactate: Early predictor of morbidity and mortality in patients with severe burns. Burns. 2005; 31(8):986-90. [DOI:10.1016/j.burns.2005.06.019] [PMID]
- Jeng JC, Jablonski K, Bridgeman A, Jordan MH. Serum lactate, not base deficit, rapidly predicts survival after major burns. Burns. 2002; 28(2):161-6. [DOI:10.1016/S0305-4179(01)00098-5] [PMID]
- Newgard CD, Rudser K, Hedges JR, Kerby JD, Stiell IG, Davis DP, et al. A critical assessment of the out-of-hospital trauma triage guidelines for physiologic abnormality. The Journal of trauma. 2010; 68(2):452-62. [DOI:10.1097/TA.0b013e3181ae20c9] [PMID]
- McNelis J, Marini CP, Jurkiewicz A, Szomstein S, Simms HH, Ritter G, et al. Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit. The American Journal of Surgery. 2001; 182(5):481-5. [DOI:10.1016/S0002-9610(01)00755-3] [PMID]
- Nasser S, Magdy AMR, EL-BARBARY A, HANAFY ABDEA. Relevance of blood lactate measurements as a marker of resuscitation in patients with severe burns. Egypt J Plast Reconstr Surg. 2008; 32:293-7.
- Rizzo JA, Rowan MP, Driscoll IR, Chung KK, Friedman BC. Vitamin C in burn resuscitation. Critical Care Clinics. 2016; 32(4):539-46. [DOI:10.1016/j.ccc.2016.06.003] [PMID]
- Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. The American Journal of Surgery. 2003; 185(5):485-91. [DOI:10.1016/S0002-9610(03)00044-8] [PMID]
- Lipsky AM, Gausche-Hill M, Henneman PL, Loffredo AJ, Eckhardt PB, Cryer HG, et al. Prehospital hypotension is a predictor of the need for an emergent, therapeutic operation in trauma patients with normal systolic blood pressure in the emergency department. The Journal of Trauma. 2006; 61(5):1228-33. [DOI:10.1097/01.ta.0000196694.52615.84] [PMID]
- Liu J, Chen X, Xu LX. New thermal wave aspects on burn evaluation of skin subjected to instantaneous heating. IEEE Transactions on Bio-Medical Engineering. 1999; 46(4):420-8. [DOI:10.1109/10.752939] [PMID]
- Holm C, Mayr M, Tegeler J, Hörbrand F, Henckel von Donnersmarck G, Mühlbauer W, et al. A clinical randomized study on the effects of invasive monitoring on burn shock resuscitation. Burns. 2004; 30(8):798-807. [DOI:10.1016/j.burns.2004.06.016] [PMID]
- Cochran A, Edelman LS, Saffle JR, Morris SE. The relationship of serum lactate and base deficit in burn patients to mortality. Journal of Burn Care & Research. 2007; 28(2):231-40. [DOI:10.1097/BCR.0B013E318031A1D1] [PMID]
- Andel D, Kamolz LP, Roka J, Schramm W, Zimpfer M, Frey M, et al. Base deficit and lactate: Early predictors of morbidity and mortality in patients with burns. Burns. 2007; 33(8):973-8. [DOI:10.1016/j.burns.2007.06.016] [PMID]
- Salehi SH, As'adi K, Mousavi J. Comparison of the outcome of burn patients using acute-phase plasma base deficit. Annals of Burns and Fire Disasters. 2011; 24(4):203-8. [PMID]
- Ibrahim I, Chor WP, Chue KM, Tan CS, Tan HL, Siddiqui FJ, et al. Is arterial base deficit still a useful prognostic marker in trauma? A systematic review. The American Journal of Emergency Medicine. 2016; 34(3):626-35. [DOI:10.1016/j.ajem.2015.12.012] [PMID]
- Mutschler M, Nienaber U, Brockamp T, Wafaisade A, Fabian T, Paffrath T, et al. Renaissance of base deficit for the initial assessment of trauma patients: A base deficit-based classification for hypovolemic shock developed on data from 16,305 patients derived from the TraumaRegister DGU®. Critical Care. 2013; 17(2):R42. [DOI:10.1186/cc12555] [PMID]
Review Paper: Research |
Subject:
General
Received: 2024/10/2 | Accepted: 2025/01/21 | Published: 2025/07/1
Received: 2024/10/2 | Accepted: 2025/01/21 | Published: 2025/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |