Volume 33, Issue 2 (6-2024)
JGUMS 2024, 33(2): 228-239 |
Back to browse issues page
Research code: IRCT20230430058033N1
Ethics code: IR.BASU.REC.1401.026
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yalfani A, Asgarpoor A. Investigating the Effects of Neurofeedback Training on Psychological Variables in Women With Non-specific Chronic Back Pain: A Randomized Controlled Trial. JGUMS 2024; 33 (2) :228-239
URL: http://journal.gums.ac.ir/article-1-2654-en.html
URL: http://journal.gums.ac.ir/article-1-2654-en.html
1- Department of Sport Injuries and Corrective Exercises, School of Sport Sciences, Bu-Ali Sina University, Hamadan, Iran.
Full-Text [PDF 4075 kb]
(382 Downloads)
| Abstract (HTML) (1597 Views)
Full-Text: (608 Views)
Introduction
Chronic low back pain (CLBP) is one of the most important medical conditions worldwide in terms of reducing quality of life, disability and increasing social and economic costs [1]. In general, CLBP has two non-specific and mechanical types. Non-specific CLBP (NSCLBP) includes 90-95% of low back pains and affects 20% of the world’s population [2, 3]. It is a complicated disease and its pathophysiology is unknown, occurring for three months or more [4]. There is strong evidence that CLBP is related to a complex interaction of cognitive [5], physical [6], psychological [7], neurophysiological [7], and lifestyle [8] factors. Although many of these factors are potentially modifiable, the CLBP rehabilitation protocols often, focus on physical interventions [9]. Physical interventions may not affect psychological factors [10]. Psychological factors not only change the activity of the cortex involved in pain processing, but also change the function of the brain areas related to attention, prediction and emotions [11].
Recently, neurofeedback training (NFBT) has attracted the attention of researchers because it provides reliable information about brain function during rest, sensory stimulation, and cognitive tasks. It is a safe, inexpensive, and noninvasive method, making it a valuable technique for clinical and research purposes [19, 20]. Despite the widespread use of neurofeedback to assess cortical changes in chronic musculoskeletal pain conditions, little is known about brain wave activity changes in CLBP patients. The results of a systematic review showed that the experience of pain is related to the activity of brain waves (EEG). In people with chronic pain such as CLBP, alpha waves decrease and beta and theta waves increase [21, 22]. Few studies have been conducted on the effect of interventions that change brain activity in people with chronic musculoskeletal pain. There are many questions in this field, the most common questions are related to the mechanism of the effectiveness of these interventions in reducing pain and how to design treatment protocols. This study aims to assess the effect of NFBT on psychological variables in women with NSCLBP.
Methods
This is a controlled clinical trial with a pre-test/post-test design. The study population includes women with NSCLBP referred to orthopedic or sports medicine clinics in Hamedan province, Iran. The G*Power software, version 3.1.9.2 was used to estimate the sample size. The software output for the sample size was 30. Considering a 10% sample dropout, it increased to 40. In this regard, 40 patients were purposefully selected and randomly divided into two groups of training and control (20 in each group). Inclusion criteria were: history of pain for more than 12 weeks, no history of spine surgery and hip joint replacement, and age 30-50 years. Exclusion criteria were: pain in other segments of the body, severe deformity of the lower and upper limbs, history of surgery, use of painkillers in the past 6 months, physical therapy in the past year, participation in sports activities, sciatica pain, spondylolysis, neuromuscular, neurological, or respiratory disorders, muscle spasm, and vertebral fracture.
The collected data were analyzed in SPSS software, version 26. At first, the Shapiro-Wilk test was used to ensure the normal distribution of the data. In addition, Levene’s test was used to check the homogeneity of variances. As a result, the analysis of covariance (ANCOVA) was used to compare the results between groups. The significance level was set at 0.05. The effect size of interventions was calculated using Cohen’s d (0.01 as small effect size, 0.06 as medium effect size and 0.14 large effect size).
Results
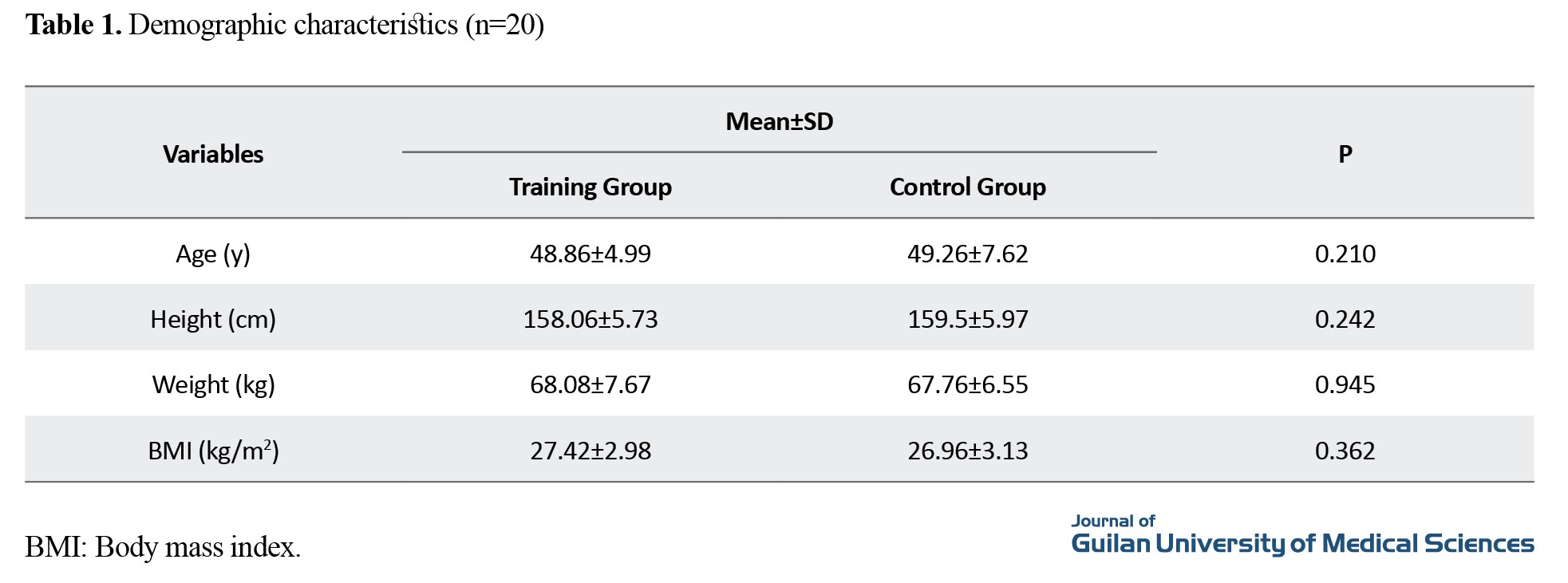
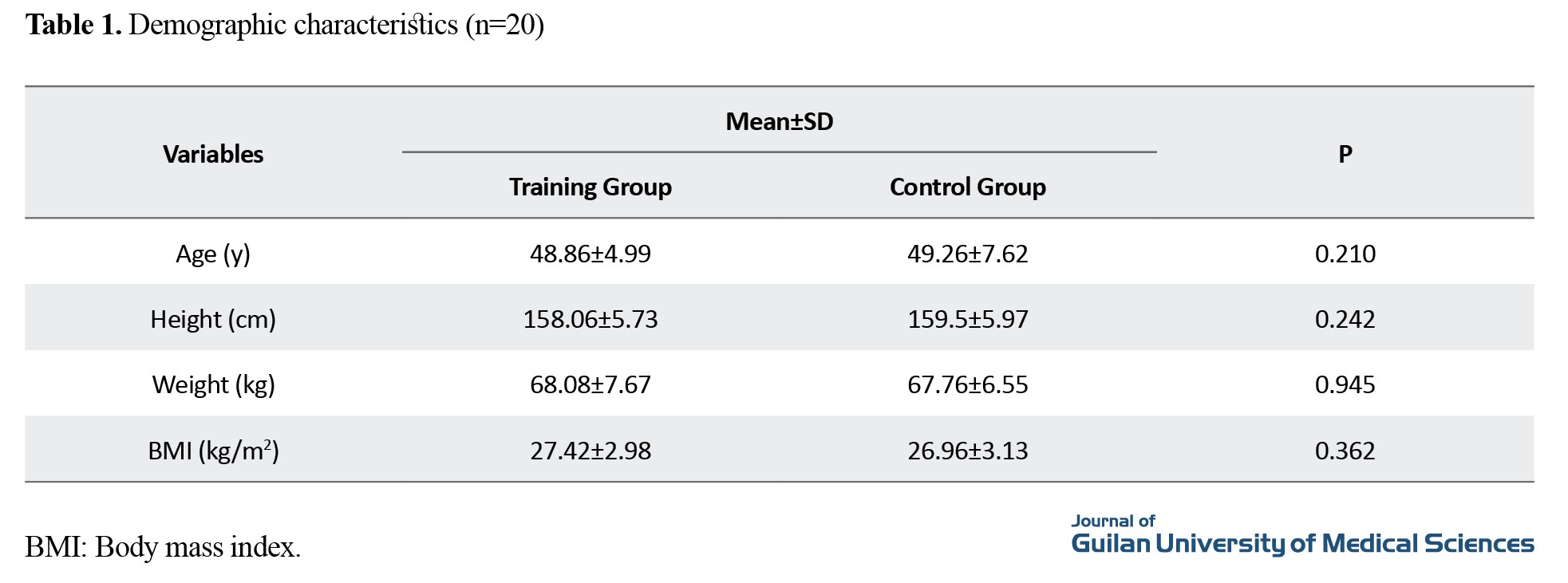
The demographic characteristics of the participants are summarized in Table 1.
The results of ANCOVA are presented in Table 2.
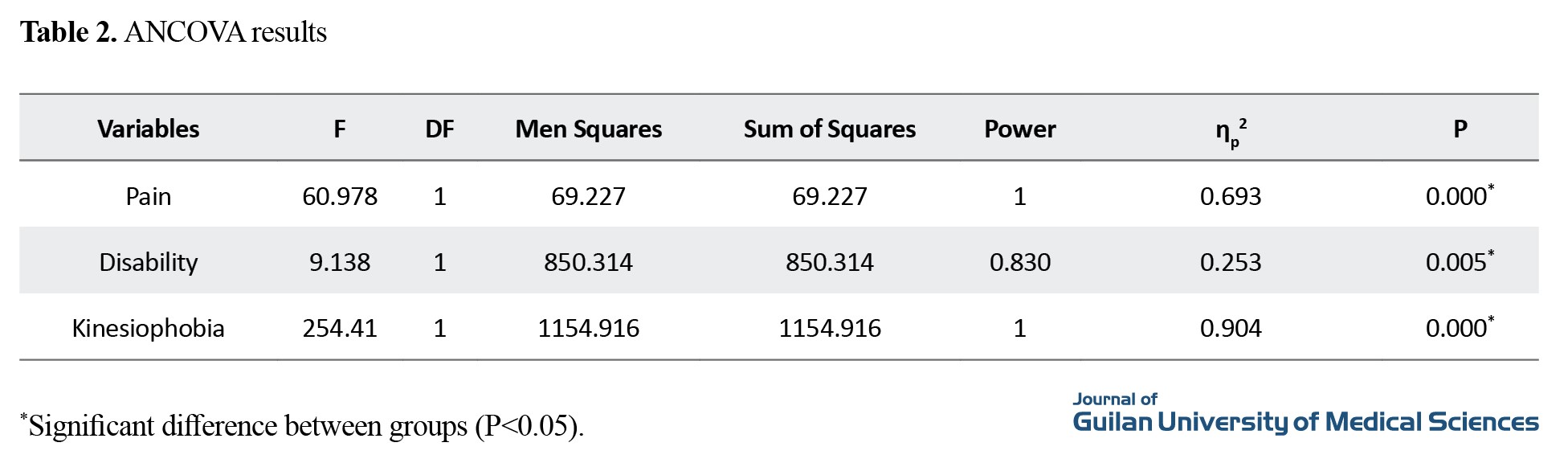
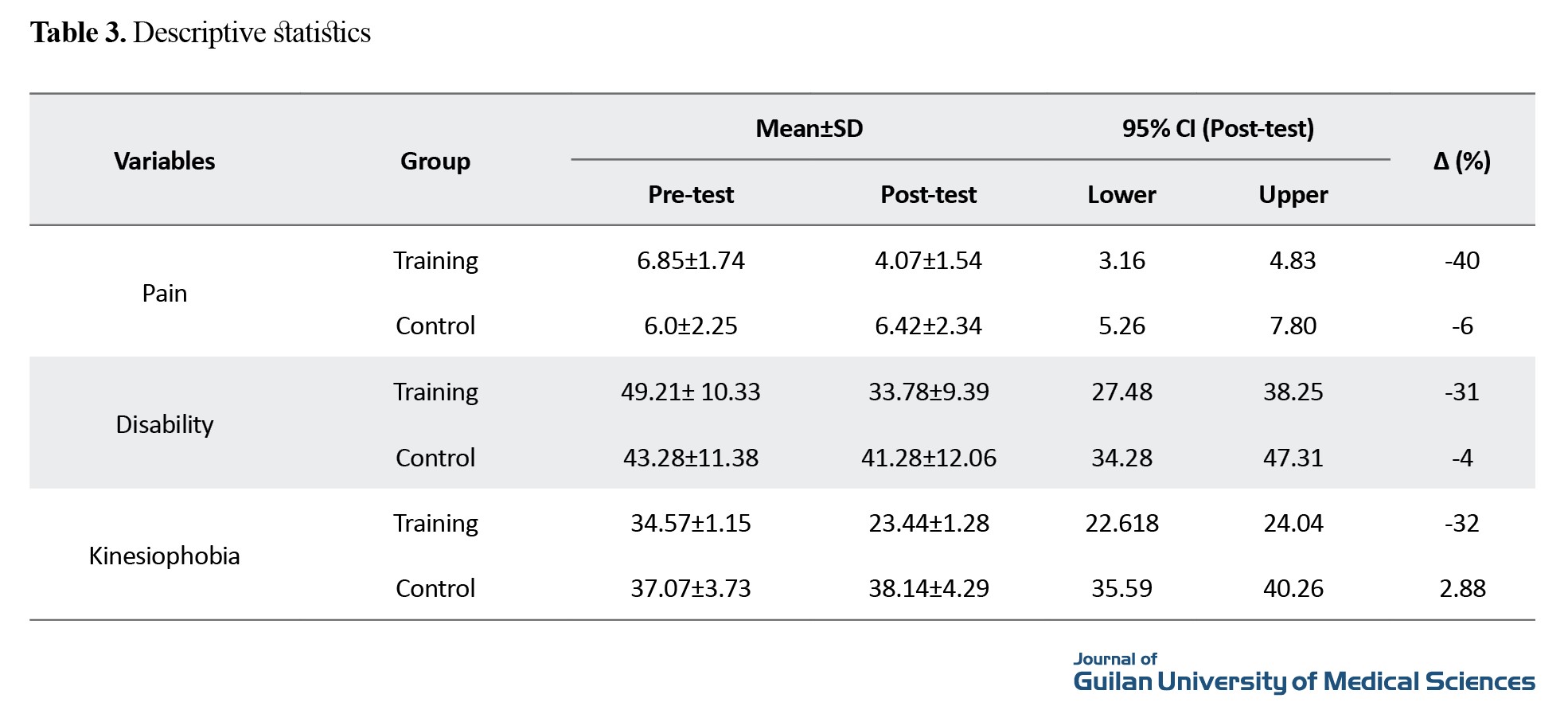
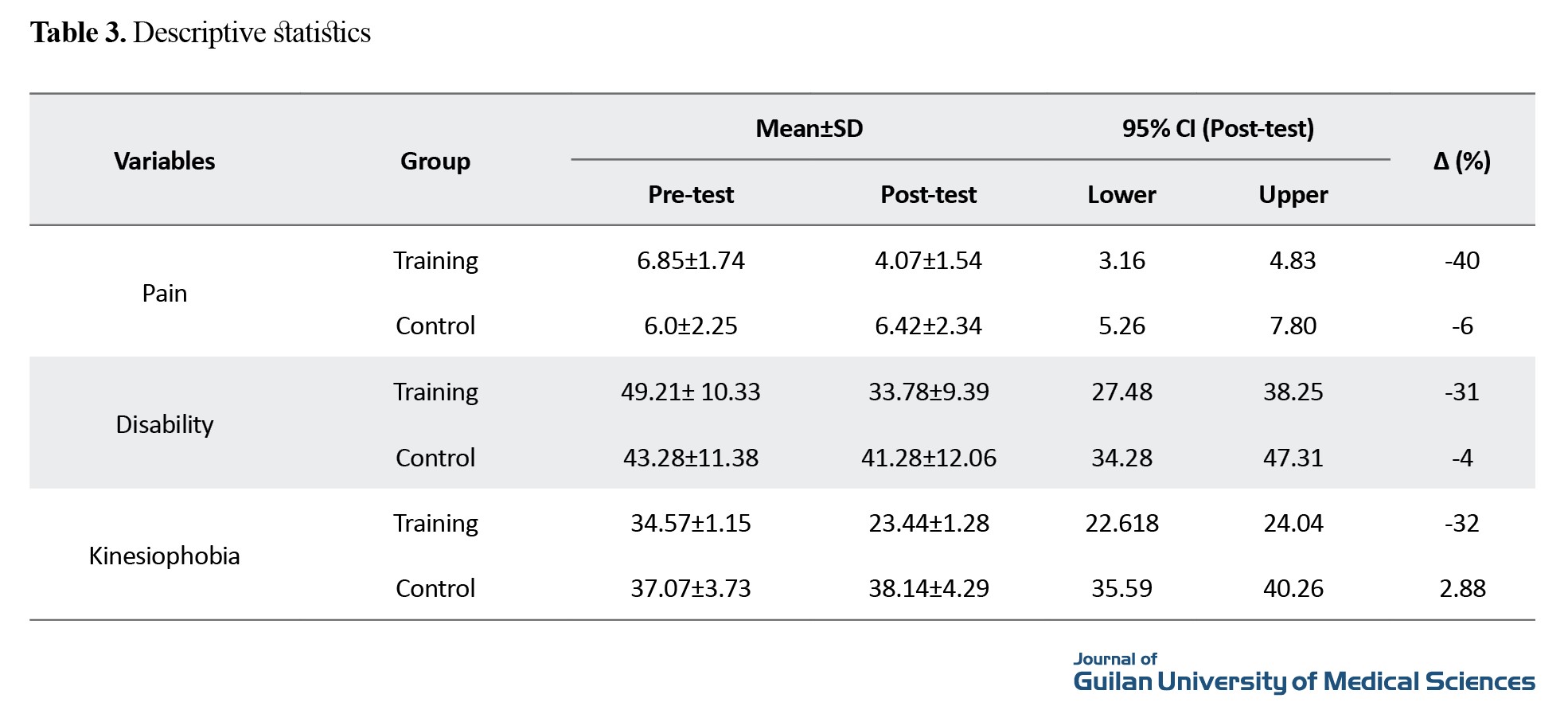
Covariance results showed that NFBT had a large significant effect on reducing pain (P=0.000, ƞ2=0.693), disability (P=0.005, ƞ2=0.253), and fear of movement (P=0.000, ƞ2=0.904) in women. In Table 3, descriptive statistics showed that the training group had a 40% reduction in pain, 31% in disability, and 32% in fear of movement.
Conclusion
The results of the present study showed a significant reduction in pain intensity, disability and fear of movement in women with NSCLBP after eight weeks of NFBT. It is recommended that rehabilitation specialists use NFBT along with physical exercises for better effectiveness in women with NSCLBP.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee Of Hamadan University of Medical Sciences, Hamadan, Iran (Code: I R.BASU.REC.1401.026).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design, data acquisition, data analysis, review and editing: Ali Yalfani; Data collection, statistics analysis and initial draft preparation: Azadeh Asgarpoor.
Conflicts of interest
The authors declared no conflict of interest.
References
Chronic low back pain (CLBP) is one of the most important medical conditions worldwide in terms of reducing quality of life, disability and increasing social and economic costs [1]. In general, CLBP has two non-specific and mechanical types. Non-specific CLBP (NSCLBP) includes 90-95% of low back pains and affects 20% of the world’s population [2, 3]. It is a complicated disease and its pathophysiology is unknown, occurring for three months or more [4]. There is strong evidence that CLBP is related to a complex interaction of cognitive [5], physical [6], psychological [7], neurophysiological [7], and lifestyle [8] factors. Although many of these factors are potentially modifiable, the CLBP rehabilitation protocols often, focus on physical interventions [9]. Physical interventions may not affect psychological factors [10]. Psychological factors not only change the activity of the cortex involved in pain processing, but also change the function of the brain areas related to attention, prediction and emotions [11].
Recently, neurofeedback training (NFBT) has attracted the attention of researchers because it provides reliable information about brain function during rest, sensory stimulation, and cognitive tasks. It is a safe, inexpensive, and noninvasive method, making it a valuable technique for clinical and research purposes [19, 20]. Despite the widespread use of neurofeedback to assess cortical changes in chronic musculoskeletal pain conditions, little is known about brain wave activity changes in CLBP patients. The results of a systematic review showed that the experience of pain is related to the activity of brain waves (EEG). In people with chronic pain such as CLBP, alpha waves decrease and beta and theta waves increase [21, 22]. Few studies have been conducted on the effect of interventions that change brain activity in people with chronic musculoskeletal pain. There are many questions in this field, the most common questions are related to the mechanism of the effectiveness of these interventions in reducing pain and how to design treatment protocols. This study aims to assess the effect of NFBT on psychological variables in women with NSCLBP.
Methods
This is a controlled clinical trial with a pre-test/post-test design. The study population includes women with NSCLBP referred to orthopedic or sports medicine clinics in Hamedan province, Iran. The G*Power software, version 3.1.9.2 was used to estimate the sample size. The software output for the sample size was 30. Considering a 10% sample dropout, it increased to 40. In this regard, 40 patients were purposefully selected and randomly divided into two groups of training and control (20 in each group). Inclusion criteria were: history of pain for more than 12 weeks, no history of spine surgery and hip joint replacement, and age 30-50 years. Exclusion criteria were: pain in other segments of the body, severe deformity of the lower and upper limbs, history of surgery, use of painkillers in the past 6 months, physical therapy in the past year, participation in sports activities, sciatica pain, spondylolysis, neuromuscular, neurological, or respiratory disorders, muscle spasm, and vertebral fracture.
The collected data were analyzed in SPSS software, version 26. At first, the Shapiro-Wilk test was used to ensure the normal distribution of the data. In addition, Levene’s test was used to check the homogeneity of variances. As a result, the analysis of covariance (ANCOVA) was used to compare the results between groups. The significance level was set at 0.05. The effect size of interventions was calculated using Cohen’s d (0.01 as small effect size, 0.06 as medium effect size and 0.14 large effect size).
Results
The demographic characteristics of the participants are summarized in Table 1.
The results of ANCOVA are presented in Table 2.
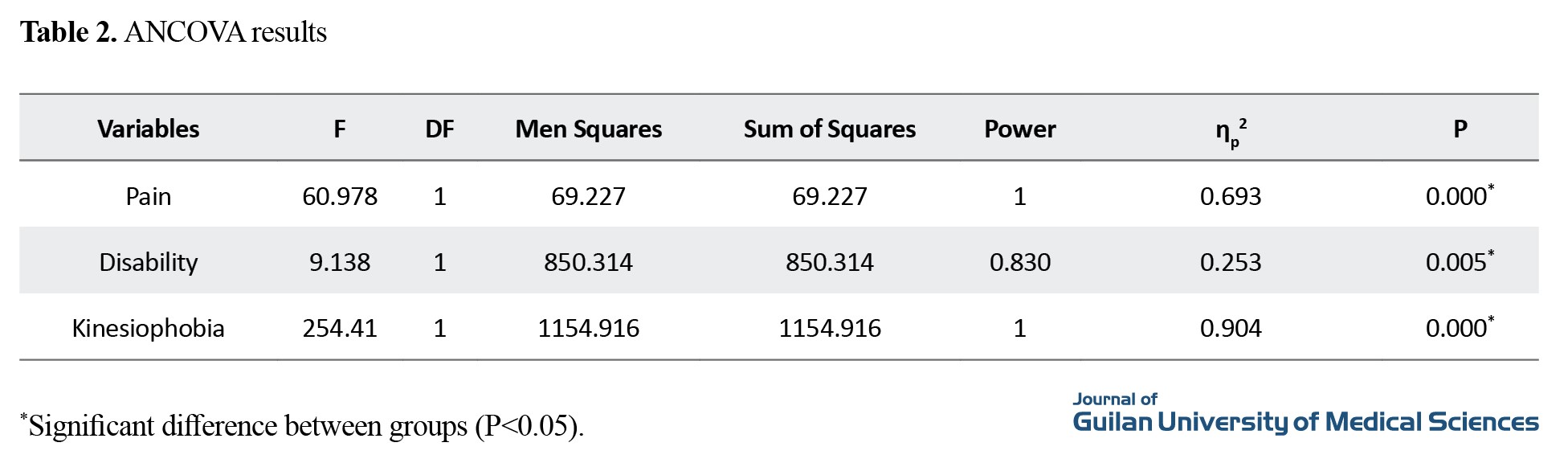
Covariance results showed that NFBT had a large significant effect on reducing pain (P=0.000, ƞ2=0.693), disability (P=0.005, ƞ2=0.253), and fear of movement (P=0.000, ƞ2=0.904) in women. In Table 3, descriptive statistics showed that the training group had a 40% reduction in pain, 31% in disability, and 32% in fear of movement.
Conclusion
The results of the present study showed a significant reduction in pain intensity, disability and fear of movement in women with NSCLBP after eight weeks of NFBT. It is recommended that rehabilitation specialists use NFBT along with physical exercises for better effectiveness in women with NSCLBP.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee Of Hamadan University of Medical Sciences, Hamadan, Iran (Code: I R.BASU.REC.1401.026).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design, data acquisition, data analysis, review and editing: Ali Yalfani; Data collection, statistics analysis and initial draft preparation: Azadeh Asgarpoor.
Conflicts of interest
The authors declared no conflict of interest.
References
- Phattharasupharerk S, Purepong N, Eksakulkla S, Siriphorn A. Effects of Qigong practice in office workers with chronic non-specific low back pain: A randomized control trial. Journal of Bodywork and Movement Therapies. 2019; 23(2):375-81. [DOI:10.1016/j.jbmt.2018.02.004] [PMID]
- Goossens N, Janssens L, Caeyenberghs K, Albouy G, Brumagne S. Differences in brain processing of proprioception related to postural control in patients with recurrent non-specific low back pain and healthy controls. NeuroImage Clinical. 2019; 23:101881. [DOI:10.1016/j.nicl.2019.101881] [PMID]
- Verbrugghe J, Agten A, Stevens S, Vandenabeele F, Roussel N, Verbunt J, et al. High intensity training improves symptoms of central sensitization at six-month follow-up in persons with chronic nonspecific low back pain: Secondary analysis of a randomized controlled trial. Brazilian Journal of Physical Therapy. 2023; 27(2):100496. [DOI:10.1016/j.bjpt.2023.100496] [PMID]
- Turci AM, Nogueira CG, Nogueira Carrer HC, Chaves TC. Self-administered stretching exercises are as effective as motor control exercises for people with chronic non-specific low back pain: A randomised trial. Journal of Physiotherapy. 2023; 69 (2):93-9. [DOI:10.1016/j.jphys.2023.02.016] [PMID]
- Campbell P, Bishop A, Dunn KM, Main CJ, Thomas E, Foster NE. Conceptual overlap of psychological constructs in low back pain. Pain. 2013; 54(9):1783-91. [DOI:10.1016/j.pain.2013.05.035] [PMID]
- Dankaerts W, O'Sullivan P, Burnett A, Straker L, Davey P, Gupta R. Discriminating healthy controls and two clinical subgroups of nonspecific chronic low back pain patients using trunk muscle activation and lumbosacral kinematics of postures and movements: A statistical classification model. Spine. 2009; 34(15):1610-8. [DOI:10.1097/BRS.0b013e3181aa6175] [PMID]
- Lee H, Hübscher M, Moseley GL, Kamper SJ, Traeger AC, Mansell G, et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain. 2015; 156(6):988-97. [DOI:10.1097/j.pain.0000000000000146] [PMID]
- Briggs AM, Jordan JE, O'Sullivan PB, Buchbinder R, Burnett AF, Osborne RH, et al. Individuals with chronic low back pain have greater di¨culty in engaging in positive lifestyle behaviours than those without back pain: An assessment of health literacy. BMC Musculoskeletal Disorders. 2011; 12:161. [DOI:10.1186/1471-2474-12-161] [PMID]
- Lack S, Neal B, De Oliveira Silva D, Barton C. How to manage patellofemoral pain-Understanding the multifactorial nature and treatment options. Physical Therapy in Sport. 2018; 32:155-66. [PMID]
- Selhorst M, Hoehn J, Degenhart T, Schmitt L, Fernandez-Fernandez A. Psychologically- informed video reduces maladaptive beliefs in adolescents with patellofemoral pain. Physical Therapy in Sport. 2020; 41:23-8. [DOI:10.1016/j.ptsp.2019.10.009] [PMID]
- Diekfuss JA, Saltman AJ, Grooms DR, Bonnette S, Foss KB, Berz K, et al. Neural correlates of knee motor control for young females with patellofemoral pain. Orthopaedic Journal of Sports Medicine. 2019; 7 (3_suppl):2325967119S0001. [DOI:10.1177/2325967119S00012]
- Kregel J, Meeus M, Malfliet A, Dolphens M, Danneels L, Nijs J, et al. Structural and functional brain abnormalities in chronic low back pain: A systematic review. Seminars in Arthritis and Rheumatism. 2015; 45(2):229-37. [DOI:10.1016/j.semarthrit.2015.05.002] [PMID]
- Diekfuss JA, Grooms DR, Coghill RC, Nissen KS, Saltman AJ, Berz K, et al. Kinesiophobia is related to brain activity for knee motor control in pediatric patients with patellofemoral pain. Orthopaedic Journal of Sports Medicine. 2020; 8(4_suppl3):2325967120S00187. [DOI:10.1177/2325967120S00187]
- Li Y, Xu Z, Xie H, Fu R, Lo WLA, Cheng X, et al. Changes in cortical activation during upright stance in individuals with chronic low back pain: An fNIRS study. Frontiers in Human Neuroscience. 2023; 17:1085831. [DOI:10.3389/fnhum.2023.1085831] [PMID]
- Apkarian AV, Sosa Y, Sonty S, Levy RM, Harden RN, Parrish TB, et al. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. Journal of Neuroscience. 2004; 24(46):10410-5. [DOI:10.1523/JNEUROSCI.2541-04.2004] [PMID]
- Giesecke T, Gracely RH, Grant MA, Nachemson A, Petzke F, Williams DA, et al. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis and Rheumatism. 2004; 50(2):613-23. [DOI:10.1002/art.20063] [PMID]
- Schouppe S, Van Oosterwijck S, Danneels L, Van Damme S, & Van Oosterwijck J. Are functional brain alterations present in low back pain? A systematic review of EEG studies. The Journal of Pain. 2020; 21(1-2):25-43. [DOI:10.1016/j.jpain.2019.06.010] [PMID]
- Gracely RH, Geisser ME, Giesecke T, Grant MA, Petzke F, Williams DA, et al. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain. 2004; 127(4):835-43. [DOI:10.1093/brain/awh098] [PMID]
- de Vries M, Wilder-Smith OH, Jongsma ML, van den Broeke EN, Arns M, van Goor H, et al. Altered resting state EEG in chronic pancreatitis patients: Toward a marker for chronic pain. Journal of Pain Research. 2013; 6:815-24. [DOI:10.2147/JPR.S50919] [PMID]
- Spronk D, Arns M, Barnett KJ, Cooper NJ, Gordon E. An investigation of EEG, genetic and cognitive markers of treatment response to antidepressant medication in patients with major depressive disorder: A pilot study. Journal of Affective Disorders. 2011; 128(1-2):41-8. [DOI:10.1016/j.jad.2010.06.021] [PMID]
- Miró J, Castarlenas E, de la Vega R, Roy R, Solé E, Tomé-Pires C, et al. Psychological neuromodulatory treatments for young people with chronic pain. Children. 2016; 3(4):41. [DOI:10.3390/children3040041] [PMID]
- Ibric VL. Neurofeedback training enhanced by light and/or electromagnetic closed-loop EEG induces analgesia in patients with neuropathic pain syndromes. Pain. 2002; 11:439-40. [Link]
- Patel K, Sutherland H, Henshaw J, Taylor JR, Brown CA, Casson AJ, et al. Effects of neurofeedback in the management of chronic pain: A systematic review and metaanalysis of clinical trials. European Journal of Pain. 2020; 24(8):1440-57.[DOI:10.1002/ejp.1612] [PMID]
- Roy R, de la Vega R, Jensen MP, Miró J. Neurofeedback for pain management: A systematic review. Frontiers in Neuroscience. 2020; 14:671. [DOI:10.3389/fnins.2020.00671] [PMID]
- Hesam-Shariati N, Chang WJ, Wewege MA, McAuley JH, Booth A, Trost Z, et al. The analgesic effect of electroencephalographic neurofeedback for people with chronic pain: A systematic review and metaanalysis. European Journal of Neurology. 2022; 29(3):921-36. [DOI:10.1111/ene.15189] [PMID]
- deCharms RC, Maeda F, Glover GH, Ludlow D, Pauly JM, Soneji D, et al. Control over brain activation and pain learned by using real-time functional MRI. Proceedings of the National Academy of Sciences of the United States of America. 2005; 102(51):18626-31. [DOI:10.1073/pnas.0505210102] [PMID]
- Armstrong K, Gokal R, Chevalier A, Todorsky W, Lim M. Microcurrent point stimulation applied to lower back acupuncture points for the treatment of nonspecific neck pain. Journal of Alternative and Complementary Medicine. 2017; 23(4):295-9. [DOI:10.1089/acm.2016.0313] [PMID]
- Inani SB, Selkar SP. Effect of core stabilization exercises versus conventional exercises on pain and functional status in patients with non-specific low back pain: A randomized clinical trial. Journal of Back and Musculoskeletal Rehabilitation. 2013; 26(1):37-43. [DOI:10.3233/BMR-2012-0348] [PMID]
- Yalfani A, Raeisi Z, Koumasian Z. Effects of eight-week water versus mat Pilates on female patients with chronic nonspecific low back pain: Double-blind randomized clinical trial. Journal of Bodywork and Movement Therapies. 2020; 24(4):70-5. [DOI:10.1016/j.jbmt.2020.06.002] [PMID]
- da Silva RA, Vieira ER, Carvalho CE, Oliveira MR, Amorim CF, Neto EN. Age-related differences on low back pain and postural control during one-leg stance: A case-control study. European Spine Journal. 2016; 25(4):1251-7. [DOI:10.1007/s00586-015-4255-9] [PMID]
- Kayıran S, Dursun E, Dursun N, Ermutlu N, Karamürsel S. Neurofeedback intervention in fibromyalgia syndrome; A randomized, controlled, rater blind clinical trial. Journal of Applied Psychophysiology and Biofeedback. 2010; 35(4):293-302. [DOI:10.1007/s10484-010-9135-9] [PMID]
- Ahmadi M, Yalfani A, Gandomi F, Rashid K. [The effect of twelve week neurofeedback training on perceptual pain, intensity, fear of pain, pelvic drop, and dynamic knee valgus index in men with patellofemoral pain syndrome: A randomized double blind clinical trial (Persian)]. Sadra Medical Journal. 2020; 8(2):151-64. [Link]
- Bismuth J, Vialatte F, Lefaucheur JP. Relieving peripheral neuropathic pain by increasing the power-ratio of low-β over high-β activities in the central cortical region with EEG-based neurofeedback: Study protocol for a controlled pilot trial (SMRPain study). Clinical Neurophysiology. 2020; 50(1):5-20. [PMID]
- Meier ML, Stämpfli P, Vrana A, Humphreys BK, Seifritz E, Hotz-Boendermaker S. Neural correlates of fear of movement in patients with chronic low back pain vs. pain-free individuals. Frontiers in Human Neuroscience. 2016; 10:386. [DOI:10.3389/fnhum.2016.00386]
- Terrasa JL, Barros-Loscertales A, Montoya P, Muñoz MA. Self-regulation of SMR power led to an enhancement of functional connectivity of somatomotor cortices in fibromyalgia patients. Frontiers in Neuroscience. 2020; 14:236. [DOI:10.3389/fnins.2020.00236] [PMID]
- Jensen MP, Day MA, Miró J. Neuromodulatory treatments for chronic pain: Efficacy and mechanisms. Nature Reviews. Neurology. 2014; 10(3):167-78. [DOI:10.1038/nrneurol.2014.12] [PMID]
- Patricio P, Roy JS, Macedo L, Roy M, Léonard G, Hodges P, et al. Repetitive transcranial magnetic stimulation alone and in combination with motor control exercise for the treatment of individuals with chronic non-specific low back pain (ExTraStim trial): Study protocol for a randomised controlled trial. BMJ Open. 2021; 11(3):e045504. [DOI:10.1136/bmjopen-2020-045504] [PMID]
Review Paper: Research |
Subject:
General
Received: 2023/10/1 | Accepted: 2023/12/24 | Published: 2024/07/1
Received: 2023/10/1 | Accepted: 2023/12/24 | Published: 2024/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |