Volume 33, Issue 3 (10-2024)
JGUMS 2024, 33(3): 346-359 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najafizadeh S R, Yaseri M. A Case Report of IgG4-related Disease With Common Clinical Manifestation in an Atypical Gender. JGUMS 2024; 33 (3) :346-359
URL: http://journal.gums.ac.ir/article-1-2698-en.html
URL: http://journal.gums.ac.ir/article-1-2698-en.html
1- Rheumatology Research Center, Vali-E-Asr Hospital, Tehran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 6584 kb]
(251 Downloads)
| Abstract (HTML) (1439 Views)
Full-Text: (562 Views)
Introduction
Immunoglobulin G4-related disease (IgG4-RD) is an immune-related condition that involves multiple organs and mimics many malignant, infectious, and inflammatory disorders [1]. The most common tissues involved are the major salivary glands, lacrimal gland, pancreas, orbits, bile ducts, and retroperitoneum. The hallmark pathological features of IgG4-RD are a lymphoplasmacytic infiltrate with a high percentage of plasma cells staining for IgG4, storiform fibrosis, obstructive phlebitis, and mild to moderate tissue eosinophilia, and the diagnosis is based on clinicopathological correlation [2].Unfortunately, the heterogeneity and ambiguity of these symptoms do not allow for clear and standardized identification and cause delays in diagnosis and treatment, which brings many problems [3]. In this study, we report two specific cases of IgG4-RD, both with retroperitoneal fibrosis.
Case Report
Case one
The first case was a 26-year-old woman with no previous medical history who visited the clinic of the hospital one month ago complaining of back pain. Her back pain was continuous and radiated to the flanks and hypogastrium. The patient complained of decreased urine output for the past two weeks, but no complaints of fever, chills, weight loss, gastrointestinal, pulmonary, or skin symptoms were recorded. Blood pressure, heart rate, body temperature, and oxygen saturation were normal at room temperature, and based on clinical examination, there was CVA tenderness in the flanks. Also, there was no peripheral lymphadenopathy in the cervical, axillary, or inguinal regions. Laboratory tests revealed a normal complete blood count (CBC), erythrocyte sedimentation rate (ESR) (40 mm/h), C-reactive protein (CRP) (10 mg/dL), blood urea nitrogen (BUN) (33 mg/dL), and creatinine (2.5 mg/dL). During the hospitalization, the patient underwent abdominal and pelvic ultrasound, which showed that the liver, gallbladder, and pancreas were normal, and no splenomegaly was found. Both kidneys were reported to be larger than normal, with the right kidney measuring 147×47 mm and the left kidney measuring 130×47 mm. Echo parenchyma of both kidneys was normal, and grade 1 hydronephrosis with ureteral dilatation was evident on both sides. Also, the ovaries and uterus were normal.
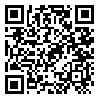
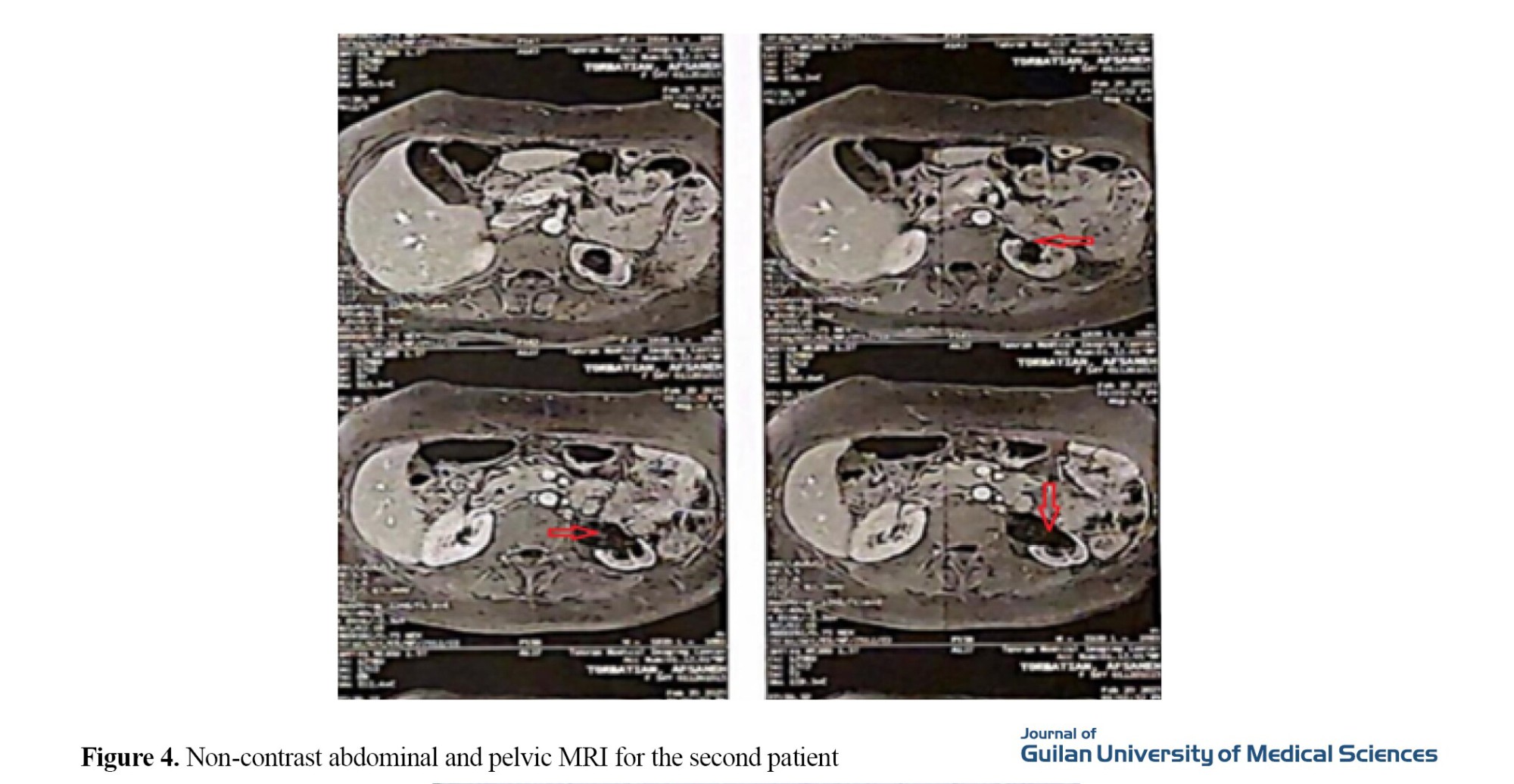
Due to hydronephrosis on ultrasound, the patient underwent a non-contrast CT scan of the abdomen and pelvis, which showed hydronephrosis without stones in the kidneys. Also, soft tissue density was observed in the para-aortic area, measuring 26×59×129 mm. Multiple lymphadenopathy with a maximum sagittal abdominal diameter (SAD) of 10 mm was observed in the abdominal cavity (Figure 1).
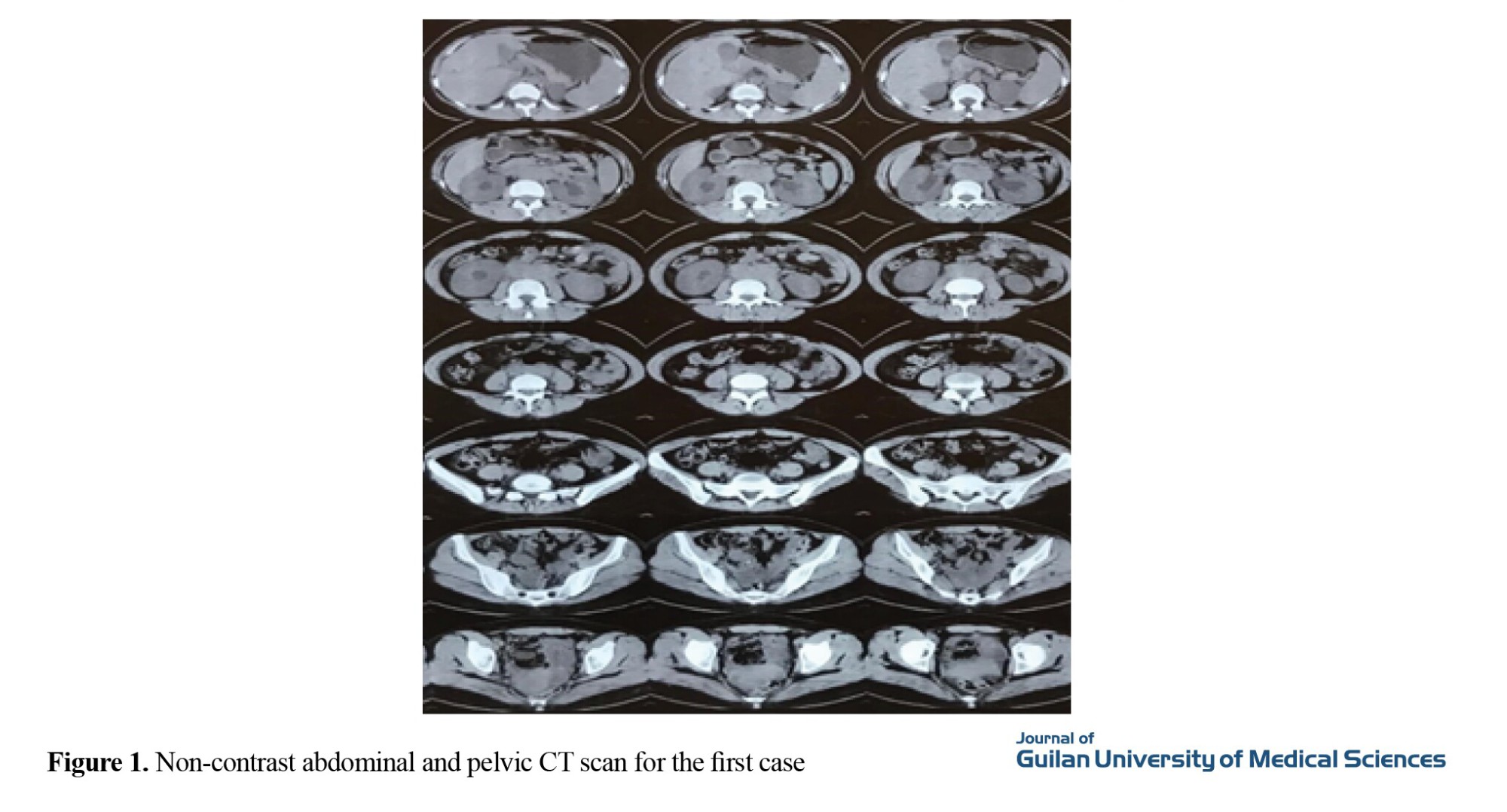
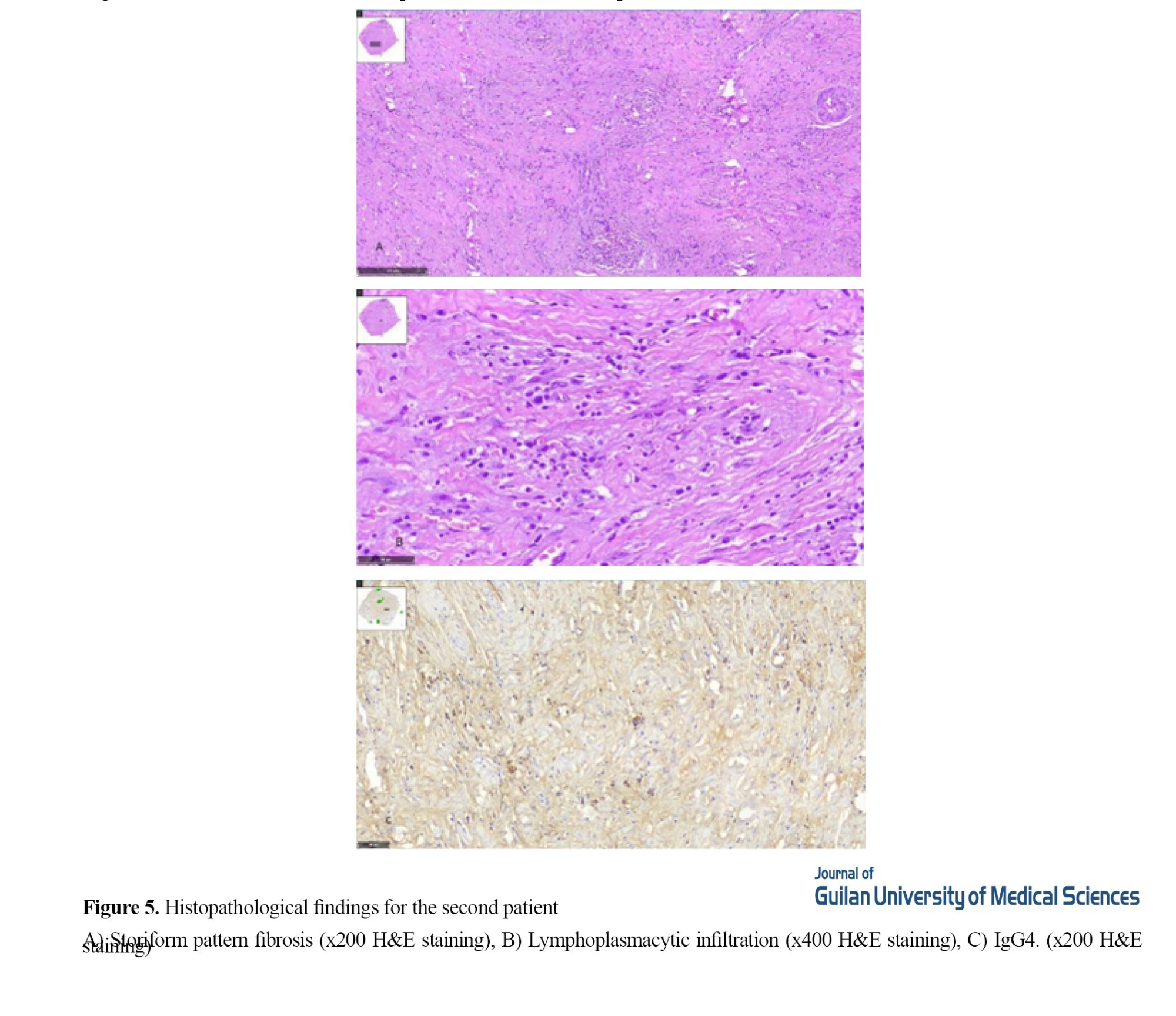
Due to increasing hydronephrosis and elevated creatinine, the patient underwent bilateral percutaneous nephrostomy (PCN). After creatinine reduction, the patient underwent non-contrast abdominal and pelvic magnetic resonance imaging (MRI), which confirmed a retroperitoneal mass around the aorta and inferior vena cava (IVC) (Figure 2).
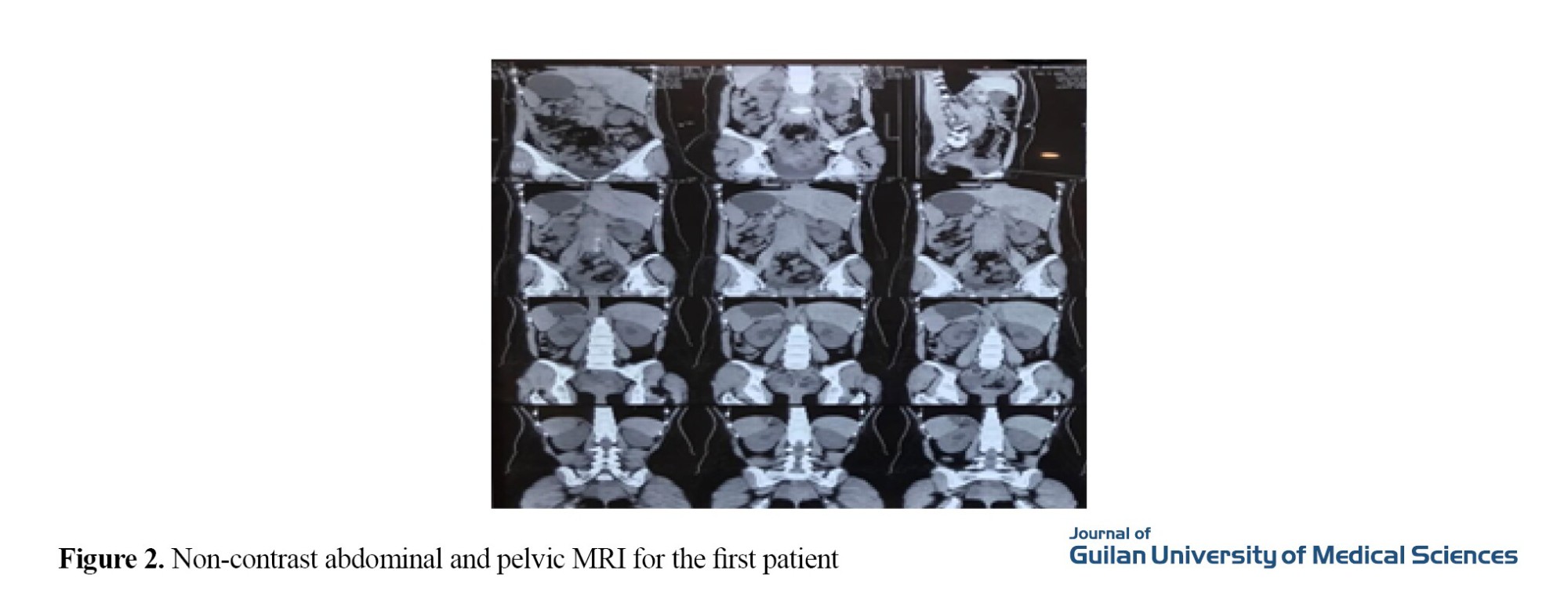
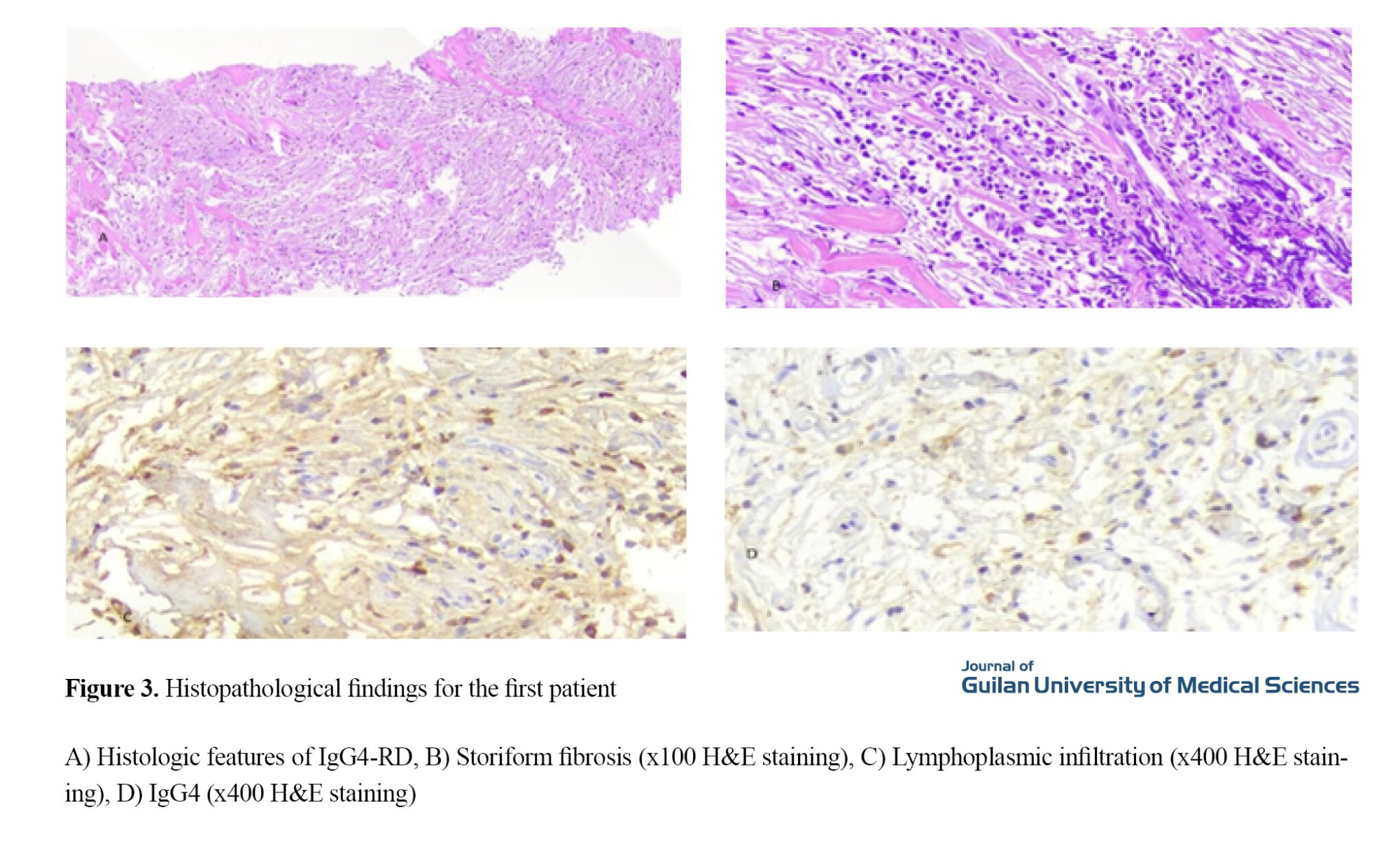
A needle biopsy of the retroperitoneal mass was performed under CT scan guidance, and pathology reports showed patchy lymphoplasmacytic infiltration between skeletal muscle fibers in the mass. In plasma cells, antigen assay results showed low CD3, low CD20, negative B-catenin, positive SMA, negative CD34, and positive IgG4 (Figure 3).
Case two
The second case was a 50-year-old woman admitted to the hospital one month ago with complaints of persistent back pain radiating to the left flank. The patient claimed that her back pain did not improve with rest and was disrupting her sleep at night. The patient also complained of decreased urine volume and had no systemic symptoms. Blood pressure, heart rate, body temperature, and oxygen saturation were normal at room temperature. On a brief physical examination, the patient had tenderness in the left flank and diffuse tenderness in the lumbar region. Laboratory evaluation showed that CBC, sodium, potassium, liver function test (LFT), ESR (55 mg/h), CRP (5 mg/dL), creatinine (1.2 mg/dL), and BUN (34 mg/dL) were normal.
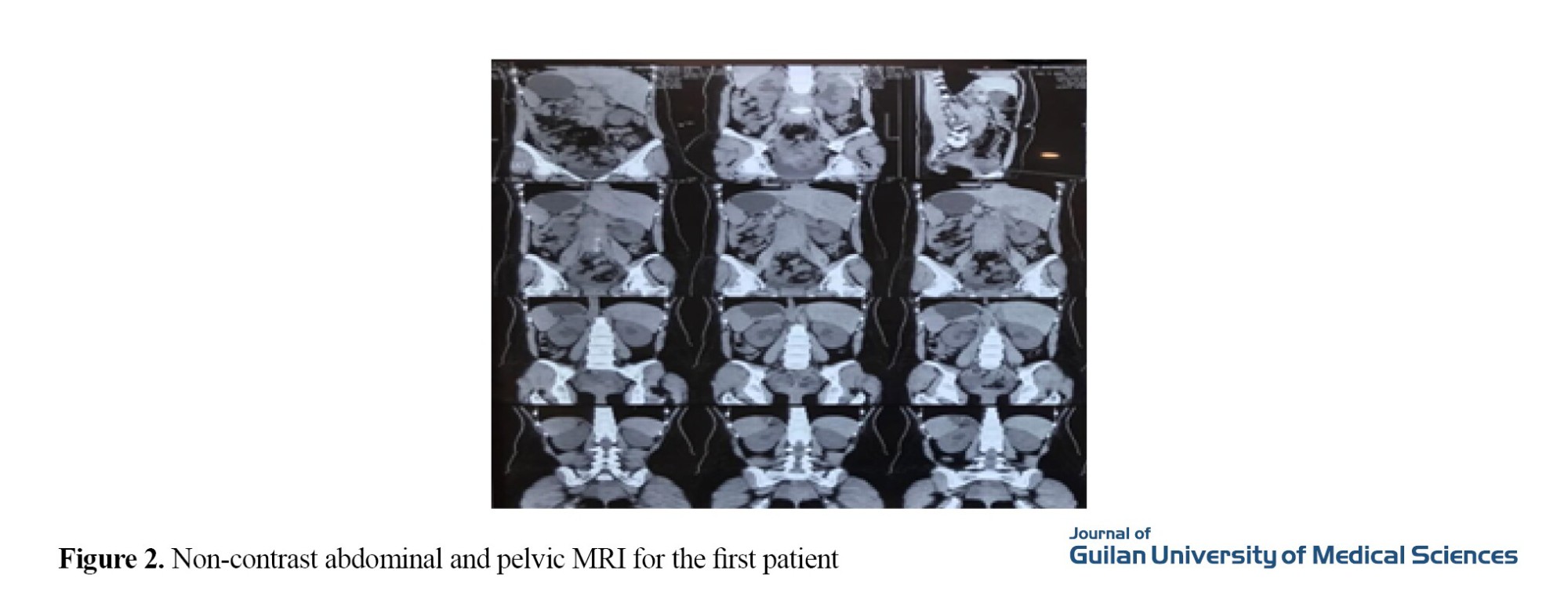
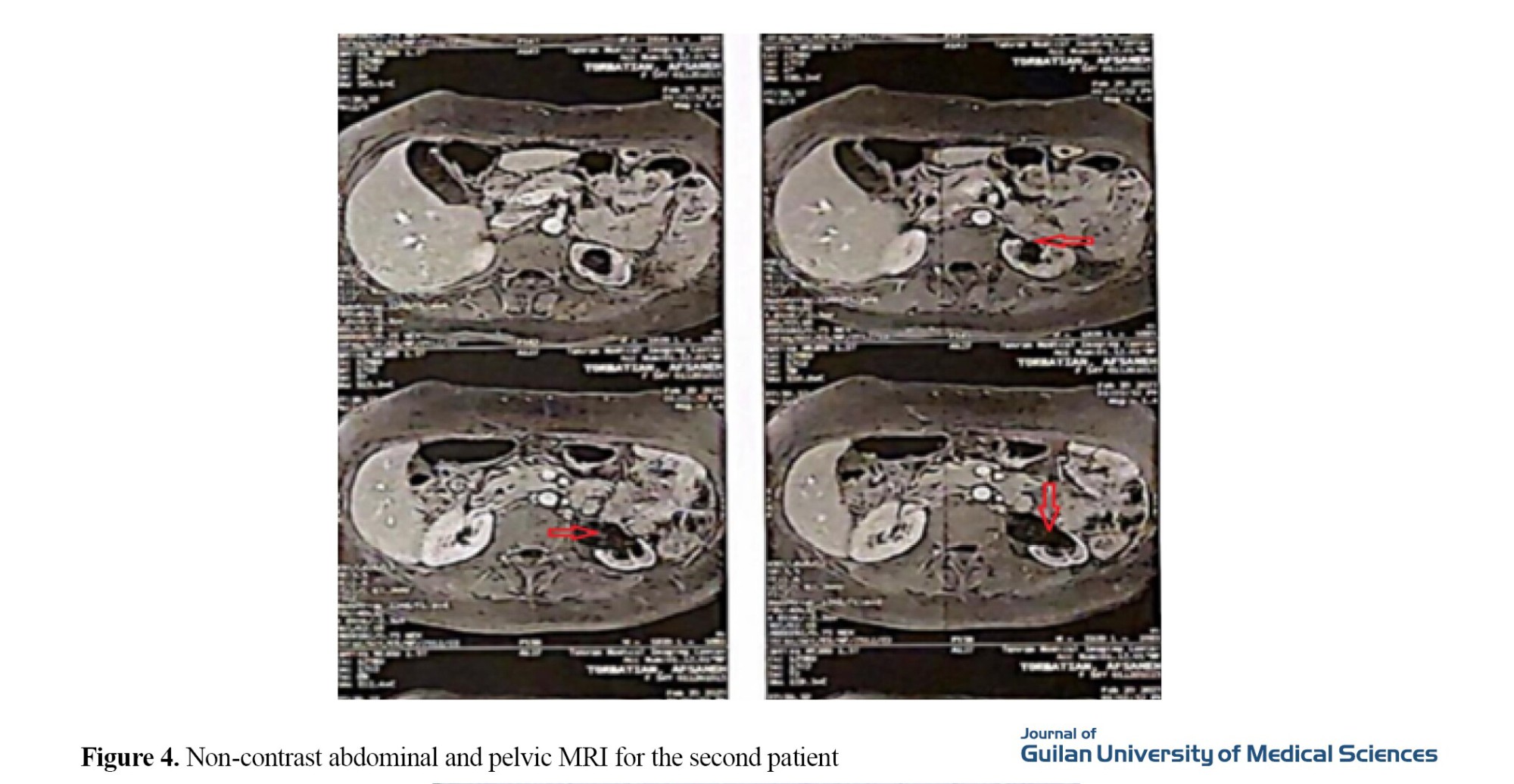
The patient underwent an ultrasound, and severe hydronephrosis was seen in the left kidney. Also, a mass measuring 19×20 mm was observed in the pelvis. Abdominal MRI showed hydronephrosis of the left kidney and a 23×19 mm mass at the pelvic inlet, which resulted in displacement of the left ureter and extension to the presacral region with retroperitoneal fibrosis. Retroperitoneal, and pelvic lymphadenopathy and mesenteric lymphadenitis were not seen (Figure 4).
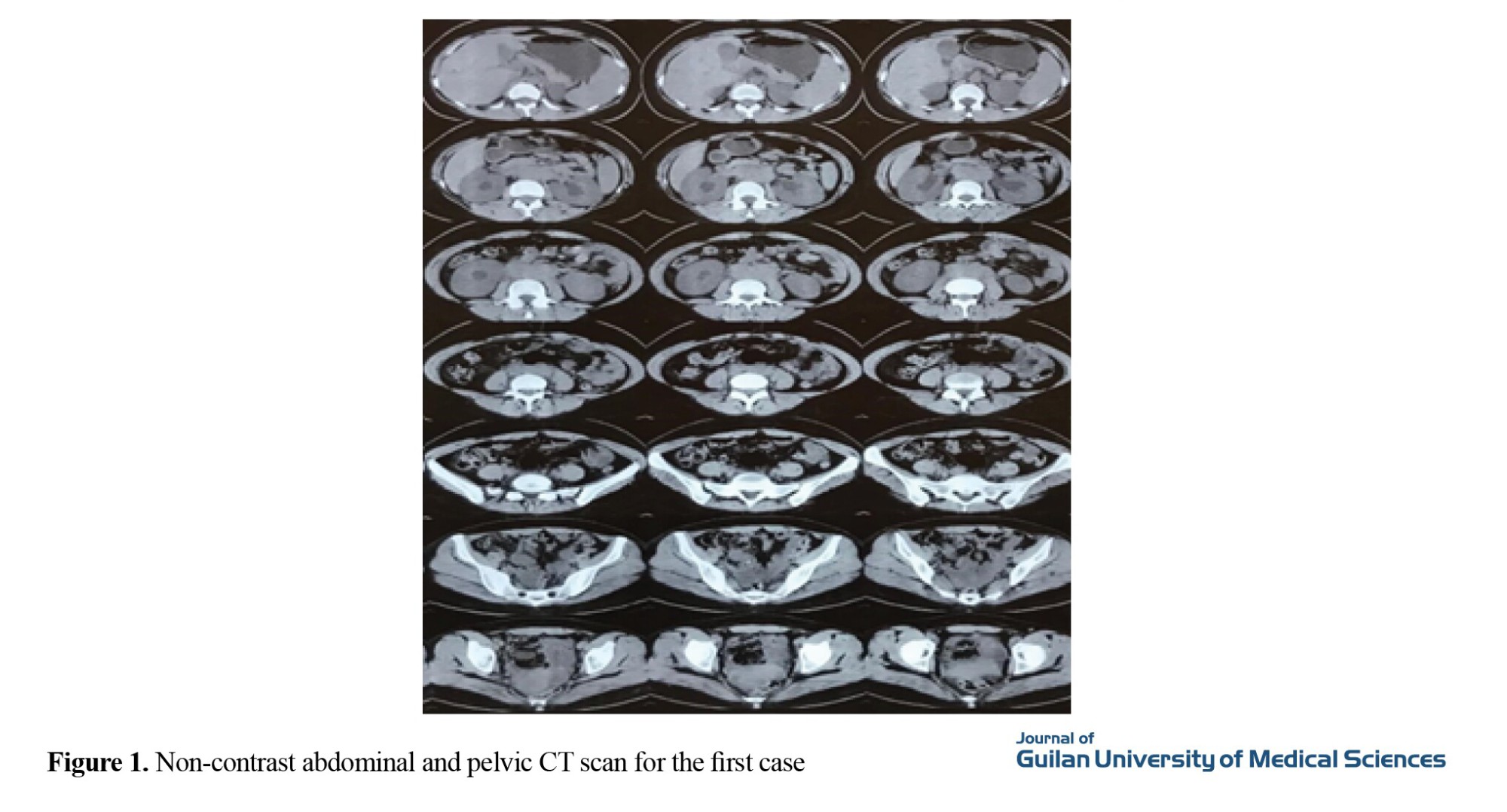
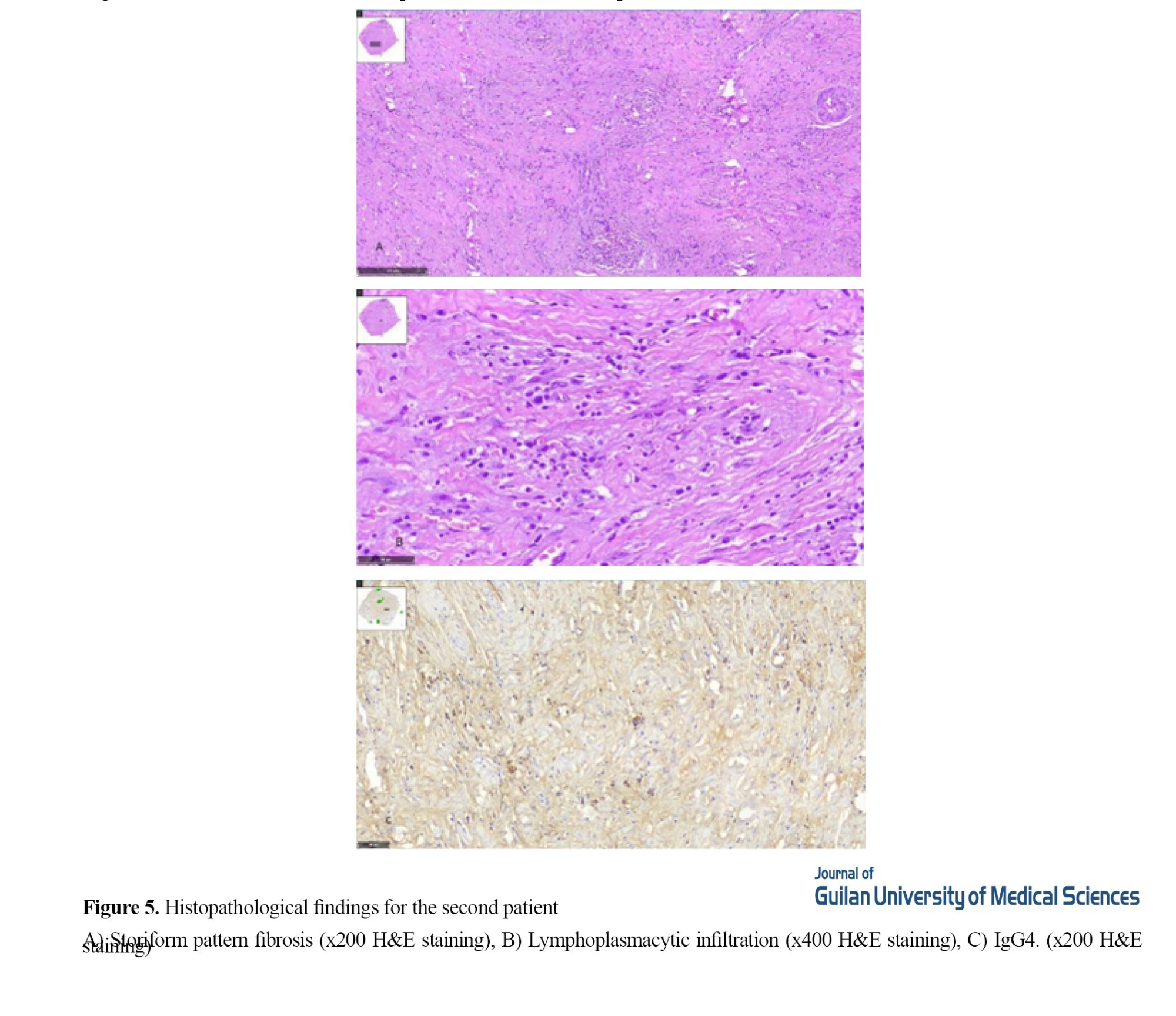
The patient then underwent a PET scan to assess possible retroperitoneal fibrosis, and mild heterogeneous F-fluorodeoxyglucose (FDG) uptake in soft tissue was observed. Then, due to increased creatinine during hospitalization and severe hydronephrosis of the left kidney, the patient underwent ureteral stenting and ureterolysis, and a biopsy was performed on the mass. The pathology report showed a retroperitoneal mass and lymphoplasmacytic infiltration in the fibroconnective tissue and ureter. On immunohistochemical (IHC) examination, IgG 4 was positive (Figure 5). Plasma cells with IgG4/IgG greater than 40% were confirmed without evidence of malignancy. IHC was negative for ALK and H-caldesmon showed normal muscle structure. The IgG level was 1850 mg/dL (700-1600 mg/dL) and the IgG4 level was 149 mg/dL (86.4-3.9 mg/dL). ANA, Anti-Ro, Anti-La and RF tests were negative.
Conclusion
The patients' complaints of lower back and flank pain should be carefully considered. Retroperitoneal mass due to IgG4-RD can be a rare, slowly progressive disease. It can have a good prognosis if diagnosed and treated promptly. The mass in our cases was periaortic, accompanied by hydronephrosis and mesenteric lymphadenitis. Both cases in our study also had involvement of the infrarenal aorta, which had a compressive effect on the ureter and led to hydronephrosis. Both patients responded well to treatment with corticosteroids and rituximab.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Ethics Committee of the University of Tehran, Tehran, Iran (Code: IR.TUNS.IKHC.REC.1402.536). Informed consent was obtained from the participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Conceptualization, methodology, validation, analysis, investigation, resources, and writing: Maryam Yaseri; Visualization, supervision, project management, review and editing: Seyed Reza Najafizadeh.
Conflicts of interest
The authors declared no conflict of interest.
References
Immunoglobulin G4-related disease (IgG4-RD) is an immune-related condition that involves multiple organs and mimics many malignant, infectious, and inflammatory disorders [1]. The most common tissues involved are the major salivary glands, lacrimal gland, pancreas, orbits, bile ducts, and retroperitoneum. The hallmark pathological features of IgG4-RD are a lymphoplasmacytic infiltrate with a high percentage of plasma cells staining for IgG4, storiform fibrosis, obstructive phlebitis, and mild to moderate tissue eosinophilia, and the diagnosis is based on clinicopathological correlation [2].Unfortunately, the heterogeneity and ambiguity of these symptoms do not allow for clear and standardized identification and cause delays in diagnosis and treatment, which brings many problems [3]. In this study, we report two specific cases of IgG4-RD, both with retroperitoneal fibrosis.
Case Report
Case one
The first case was a 26-year-old woman with no previous medical history who visited the clinic of the hospital one month ago complaining of back pain. Her back pain was continuous and radiated to the flanks and hypogastrium. The patient complained of decreased urine output for the past two weeks, but no complaints of fever, chills, weight loss, gastrointestinal, pulmonary, or skin symptoms were recorded. Blood pressure, heart rate, body temperature, and oxygen saturation were normal at room temperature, and based on clinical examination, there was CVA tenderness in the flanks. Also, there was no peripheral lymphadenopathy in the cervical, axillary, or inguinal regions. Laboratory tests revealed a normal complete blood count (CBC), erythrocyte sedimentation rate (ESR) (40 mm/h), C-reactive protein (CRP) (10 mg/dL), blood urea nitrogen (BUN) (33 mg/dL), and creatinine (2.5 mg/dL). During the hospitalization, the patient underwent abdominal and pelvic ultrasound, which showed that the liver, gallbladder, and pancreas were normal, and no splenomegaly was found. Both kidneys were reported to be larger than normal, with the right kidney measuring 147×47 mm and the left kidney measuring 130×47 mm. Echo parenchyma of both kidneys was normal, and grade 1 hydronephrosis with ureteral dilatation was evident on both sides. Also, the ovaries and uterus were normal.
Due to hydronephrosis on ultrasound, the patient underwent a non-contrast CT scan of the abdomen and pelvis, which showed hydronephrosis without stones in the kidneys. Also, soft tissue density was observed in the para-aortic area, measuring 26×59×129 mm. Multiple lymphadenopathy with a maximum sagittal abdominal diameter (SAD) of 10 mm was observed in the abdominal cavity (Figure 1).
Due to increasing hydronephrosis and elevated creatinine, the patient underwent bilateral percutaneous nephrostomy (PCN). After creatinine reduction, the patient underwent non-contrast abdominal and pelvic magnetic resonance imaging (MRI), which confirmed a retroperitoneal mass around the aorta and inferior vena cava (IVC) (Figure 2).
A needle biopsy of the retroperitoneal mass was performed under CT scan guidance, and pathology reports showed patchy lymphoplasmacytic infiltration between skeletal muscle fibers in the mass. In plasma cells, antigen assay results showed low CD3, low CD20, negative B-catenin, positive SMA, negative CD34, and positive IgG4 (Figure 3).
Case two
The second case was a 50-year-old woman admitted to the hospital one month ago with complaints of persistent back pain radiating to the left flank. The patient claimed that her back pain did not improve with rest and was disrupting her sleep at night. The patient also complained of decreased urine volume and had no systemic symptoms. Blood pressure, heart rate, body temperature, and oxygen saturation were normal at room temperature. On a brief physical examination, the patient had tenderness in the left flank and diffuse tenderness in the lumbar region. Laboratory evaluation showed that CBC, sodium, potassium, liver function test (LFT), ESR (55 mg/h), CRP (5 mg/dL), creatinine (1.2 mg/dL), and BUN (34 mg/dL) were normal.
The patient underwent an ultrasound, and severe hydronephrosis was seen in the left kidney. Also, a mass measuring 19×20 mm was observed in the pelvis. Abdominal MRI showed hydronephrosis of the left kidney and a 23×19 mm mass at the pelvic inlet, which resulted in displacement of the left ureter and extension to the presacral region with retroperitoneal fibrosis. Retroperitoneal, and pelvic lymphadenopathy and mesenteric lymphadenitis were not seen (Figure 4).
The patient then underwent a PET scan to assess possible retroperitoneal fibrosis, and mild heterogeneous F-fluorodeoxyglucose (FDG) uptake in soft tissue was observed. Then, due to increased creatinine during hospitalization and severe hydronephrosis of the left kidney, the patient underwent ureteral stenting and ureterolysis, and a biopsy was performed on the mass. The pathology report showed a retroperitoneal mass and lymphoplasmacytic infiltration in the fibroconnective tissue and ureter. On immunohistochemical (IHC) examination, IgG 4 was positive (Figure 5). Plasma cells with IgG4/IgG greater than 40% were confirmed without evidence of malignancy. IHC was negative for ALK and H-caldesmon showed normal muscle structure. The IgG level was 1850 mg/dL (700-1600 mg/dL) and the IgG4 level was 149 mg/dL (86.4-3.9 mg/dL). ANA, Anti-Ro, Anti-La and RF tests were negative.
Conclusion
The patients' complaints of lower back and flank pain should be carefully considered. Retroperitoneal mass due to IgG4-RD can be a rare, slowly progressive disease. It can have a good prognosis if diagnosed and treated promptly. The mass in our cases was periaortic, accompanied by hydronephrosis and mesenteric lymphadenitis. Both cases in our study also had involvement of the infrarenal aorta, which had a compressive effect on the ureter and led to hydronephrosis. Both patients responded well to treatment with corticosteroids and rituximab.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval was obtained from the Ethics Committee of the University of Tehran, Tehran, Iran (Code: IR.TUNS.IKHC.REC.1402.536). Informed consent was obtained from the participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors' contributions
Conceptualization, methodology, validation, analysis, investigation, resources, and writing: Maryam Yaseri; Visualization, supervision, project management, review and editing: Seyed Reza Najafizadeh.
Conflicts of interest
The authors declared no conflict of interest.
References
- Perugino CA, Mattoo H, Mahajan VS, Maehara T, Wallace ZS, Pillai S, et al. Emerging treatment models in rheumatology: IgG4‐related disease: Insights into human immunology and targeted therapies. Arthritis & Rheumatology (Hoboken, N.J.). 2017; 69(9):1722-32. [DOI:10.1002/art.40168] [PMID] [PMCID]
- Zen Y, Nakanuma Y. IgG4-related disease: A cross-sectional study of 114 cases.The American Journal of Surgical Pathology. 2010; 34(12):1812-9. [DOI:10.1097/PAS.0b013e3181f7266b] [PMID]
- Comai G, Cuna V, Fabbrizio B, Sabattini E, Leone O, Tondolo F, et al. A case report of IgG4-related disease: An insidious path to the diagnosis through kidney, heart and brain. BMC Nephrology. 2019; 20(1):418. [DOI:10.1186/s12882-019-1587-4] [PMID] [PMCID]
- Lian L, Wang C, Tian JL. IgG4‐related retroperitoneal fibrosis: A newly characterized disease. International Journal of Rheumatic Diseases. 2016; 19(11):1049-55. [DOI:10.1111/1756-185X.12863] [PMID]
- Bangolo AI, Gupta K, Atoot A. IgG4-Related disease retroperitoneal fibrosis: An unusual cause of low back pain. Cureus. 2021; 13(2):e13608. [DOI:10.7759/cureus.13608] [PMID] [PMCID]
- Gormley S, Bravo PT, Kos X, Solanki K, Khashram M. A case of IgG4-related retroperitoneal fibrosis with significant involvement of the abdominal aorta-a clinical and diagnostic challenge. Journal of Vascular Surgery Cases and Innovative Techniques. 2022; 8(2):275-80. [DOI:10.1016/j.jvscit.2022.02.003] [PMID] [PMCID]
- Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. Journal of Gastroenterology. 2003; 38(10):982-4.[DOI:10.1007/s00535-003-1175-y] [PMID]
- Nikiphorou E, Galloway J, Fragoulis GE. Overview of IgG4-related aortitis and periaortitis. A decade since their first description. Autoimmunity Reviews. 2020; 19(12):102694. [DOI:10.1016/j.autrev.2020.102694] [PMID]
- Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, et al. International consensus guidance statement on the management and treatment of IgG4‐related disease. Arthritis & Rheumatology. 2015; 67(7):1688-99. [DOI:10.1002/art.39132] [PMID]
- Mota MMDS, Bezerra ROF, Garcia MRT. Practical approach to primary retroperitoneal masses in adults. Radiologia Brasileira. 2018; 51(6):391-400. [DOI:10.1590/0100-3984.2017.0179] [PMID] [PMCID]
- Almeqdadi M, Al-Dulaimi M, Perepletchikov A, Tomera K, Jaber BL. Rituximab for retroperitoneal fibrosis due to IgG4-related disease: A case report and literature review. Clinical Nephrology. 2018; 6:4-10. [DOI:10.5414/CNCS109321] [PMID] [PMCID]
Review Paper: Case report |
Subject:
Special
Received: 2024/04/13 | Accepted: 2024/04/23 | Published: 2024/10/1
Received: 2024/04/13 | Accepted: 2024/04/23 | Published: 2024/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |