Volume 33, Issue 2 (6-2024)
JGUMS 2024, 33(2): 240-253 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shokri B, Bagheri Bavandpouri S R, Asadzade S, Alimohammadi E. Investigating the Factors Associated With Poor Clinical Outcomes of Children With Moderate to Severe Traumatic Brain Injury: A Retrospective Observational Study. JGUMS 2024; 33 (2) :240-253
URL: http://journal.gums.ac.ir/article-1-2622-en.html
URL: http://journal.gums.ac.ir/article-1-2622-en.html
1- Clinical Research Development Center, Taleghani Hospitals, Imam Ali Hospitals, Kermanshah University of Medical Sciences, Kermanshah,Iran.
2- Department of Neurosurgery, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran.
3- Medical doctor, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- Department of Neurosurgery, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran.
3- Medical doctor, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran.
Full-Text [PDF 3199 kb]
(377 Downloads)
| Abstract (HTML) (1990 Views)
Full-Text: (491 Views)
Introduction
Traumatic brain injury (TBI) is one of the main causes of death and disability in children [10, 11]. This type of injury occurs due to a blow to the head, caused by falling, car accidents, sports accidents, etc. The TBI can lead to undesirable clinical outcomes that affect the lives of children and their families. It can be divided into primary and secondary injuries [14, 15]. The primary TBI is an irreversible event defined as direct physical injury to the brain such as compression, displacement, deformation, shearing, tearing, or crushing of brain and blood vessels [2]. The secondary TBI is an indirect injury to the head caused by neurological cascades of events that can eventually lead to the neuronal cell death [16]. To improve the optimal forecasting and management of TBI in children, it is important to understand the factors associated with adverse clinical consequences. Many studies in the field of TBI have been conducted on adults; there is scant research on children and adolescents. In this study, we aim to examine the factors associated with adverse clinical consequences of TBI in children with moderate to severe TBI.
Methods
In this study, all children and adolescents (aged ≤18 years) with moderate to severe TBI (based on the Classification System for TBI Severity) [10] referred to our center from May 2013 to June 2020 were evaluated. The entry criteria were the occurrence of TBI, a Glasgow coma scale (GCS) score ≤13 [3], and age <18. Those with death due to non-brain injuries in the first 24 hours were excluded from the study. Demographic, clinical, radiology and laboratory data were investigated. These data included: age, sex, cause of trauma, GCS at the time of admission, pupil reaction to light, Rotterdam computer tomography (CT) score, hospitalization length, anemia during admission, and high blood sugar during admission. All patients were managed in accordance with the advanced trauma life support protocol for severe head injury where mass lesions are discharged with surgery and all unconscious patients with GCS≤8 are intubated and underwent mechanical ventilation [19].
All patients underwent CT scanning at the time of admission. The CT scans were classified by the main author retrospectively based on the Rotterdam classification system [20]. The clinical outcomes at the time of discharge from the hospital were evaluated using the Glasgow outcome scale (GOS) [7]. This scale grades the outcomes as 5= good recovery; 4= moderate disability; 3= severe disability; 2= persistent vegetative; and 1= death. The data was analyzed using SPSS software, version 23 (SPSS Inc. Chicago, Illinois). Descriptive statistics were reported as median (range) for continuous variables and frequency (percentage) for discrete variables. We used the Chi-Square test or Fisher's exact test to evaluate the difference between ratios. The student T-test was used to evaluate continuous variables. Binary logistic regression analysis was used to evaluate the independent relationship between different variables and clinical results. P<0.05 was considered statistically significant.
Results
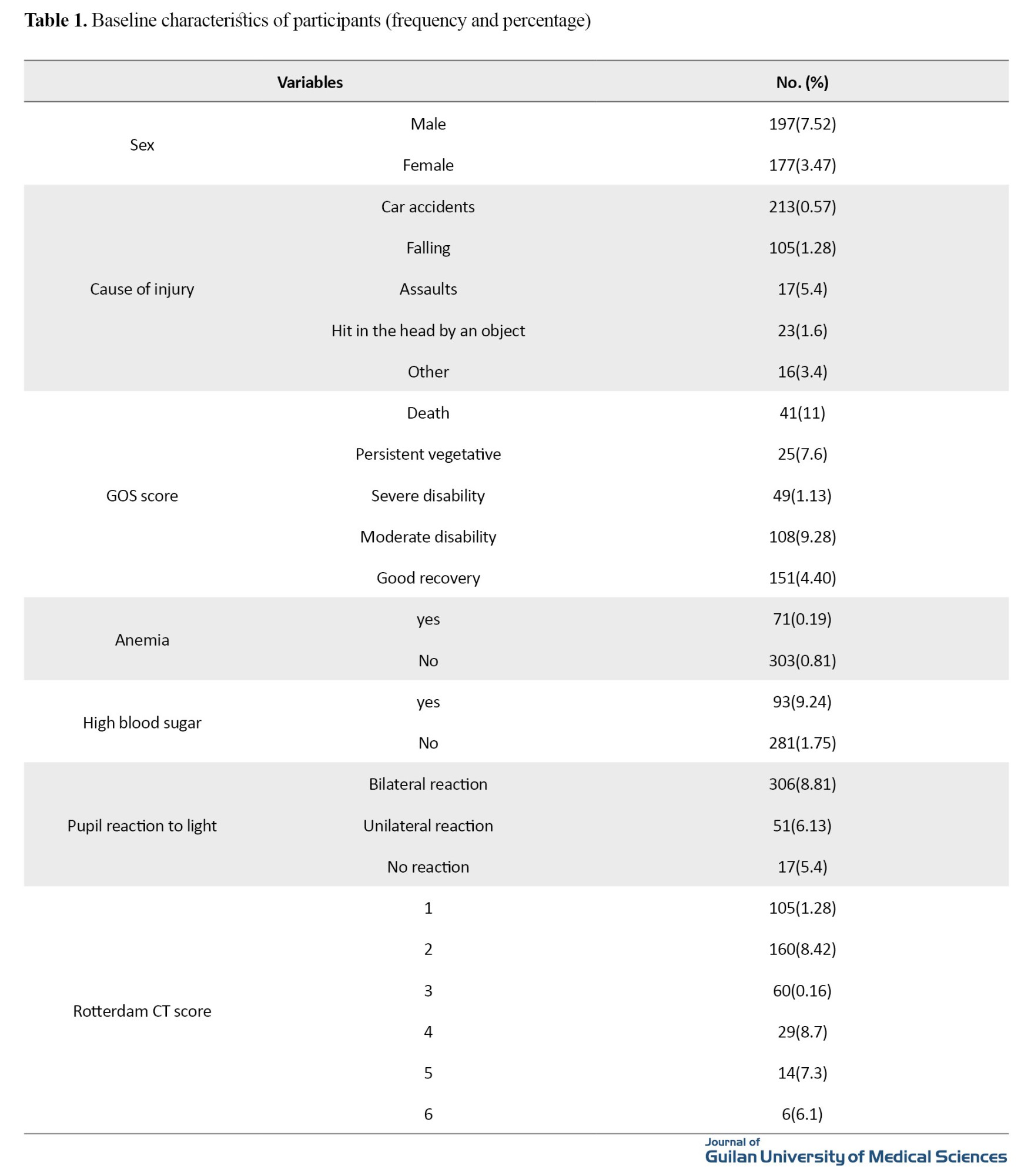
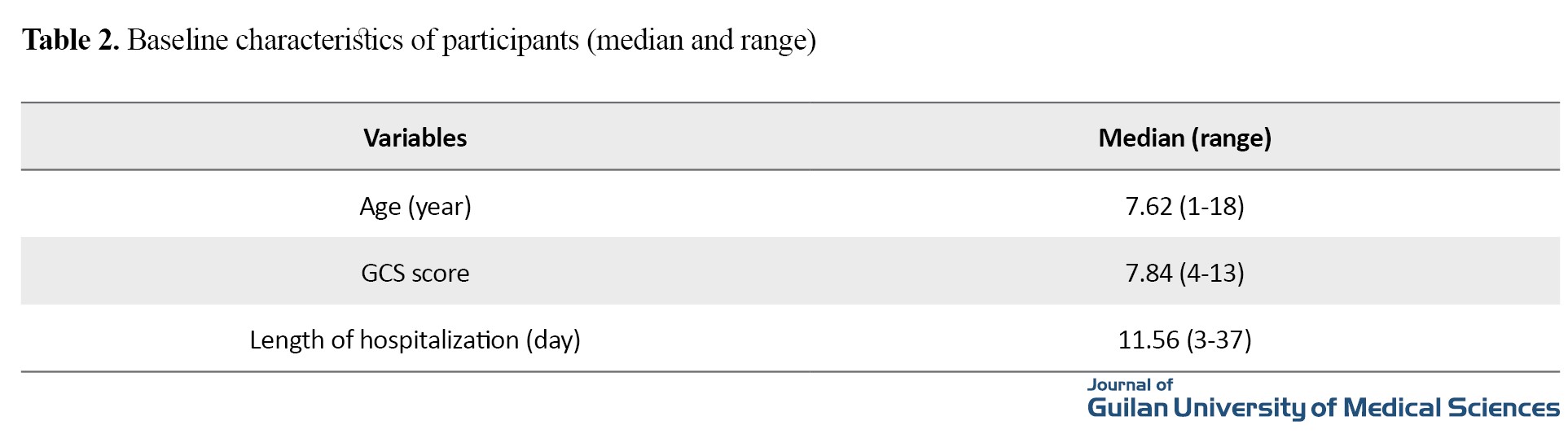
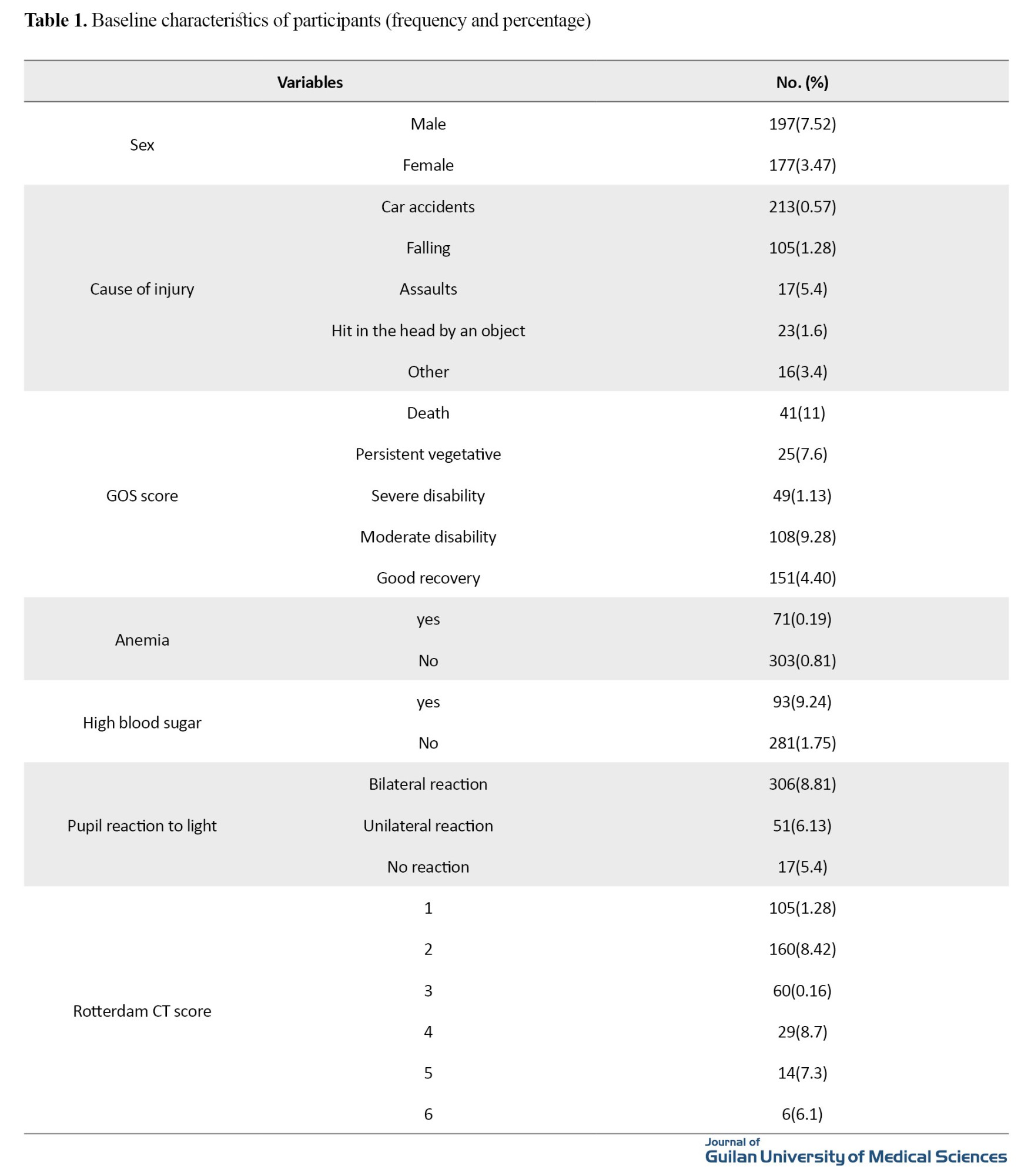
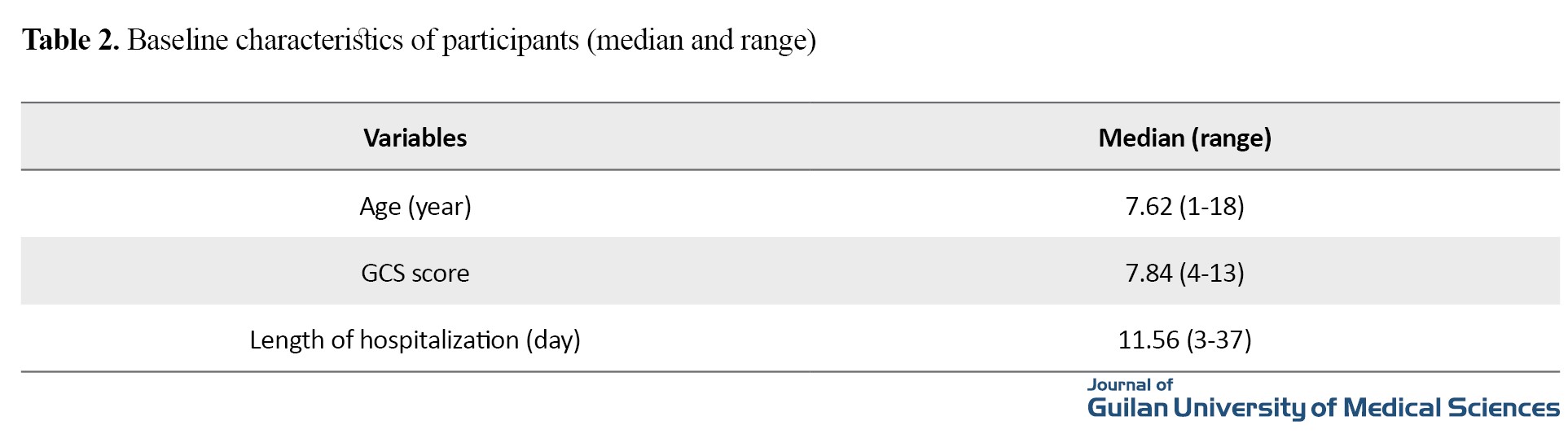
In this study, 374 children with moderate to severe TBI were evaluated, of whom 197 (52.7%) were boys and 177 (47.3%) were girls. Their mean age during injury was 7.37±3.11 years. The baseline characteristics of patients are shown in tables 1 and 2.
The univariate regression analysis showed that the GCS score, pupillary light reflex, the Rotterdam CT score, anemia during admission, and high blood sugar during admission were associated with adverse outcomes of TBI in children (P<0.05). Multiple regression analysis results showed the GCS score (OR=3.2; 95% CI: 1.78-5.24; P<0.001), pupillary light reflex (OR=1.97; 95% CI: 1.34-2.99; P=0.024), and the Rotterdam CT score (OR=2.61; 95% CI: 1.72-4.13; P=0.020) had a relationship with clinical outcomes.
Conclusion
The GCS score, pupillary light reflex, and the Rotterdam CT score can predict adverse clinical outcomes in children with moderate to severe TBI. The results of this study can be used to improve the management of these patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1399.248).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Methodology, supervision: Ehsan Alimohammadi and Seyed Reza Bagheri Bavandpouri; Data collection: Sahel Asadzade and Bita Shokri; Initial draft preparation: Bita Shokri and Ehsan Alimohammadi; Conceptualization, investigation, editing & review: All authors.
Conflicts of interest
The authors declare no conflict of interest.
References
Traumatic brain injury (TBI) is one of the main causes of death and disability in children [10, 11]. This type of injury occurs due to a blow to the head, caused by falling, car accidents, sports accidents, etc. The TBI can lead to undesirable clinical outcomes that affect the lives of children and their families. It can be divided into primary and secondary injuries [14, 15]. The primary TBI is an irreversible event defined as direct physical injury to the brain such as compression, displacement, deformation, shearing, tearing, or crushing of brain and blood vessels [2]. The secondary TBI is an indirect injury to the head caused by neurological cascades of events that can eventually lead to the neuronal cell death [16]. To improve the optimal forecasting and management of TBI in children, it is important to understand the factors associated with adverse clinical consequences. Many studies in the field of TBI have been conducted on adults; there is scant research on children and adolescents. In this study, we aim to examine the factors associated with adverse clinical consequences of TBI in children with moderate to severe TBI.
Methods
In this study, all children and adolescents (aged ≤18 years) with moderate to severe TBI (based on the Classification System for TBI Severity) [10] referred to our center from May 2013 to June 2020 were evaluated. The entry criteria were the occurrence of TBI, a Glasgow coma scale (GCS) score ≤13 [3], and age <18. Those with death due to non-brain injuries in the first 24 hours were excluded from the study. Demographic, clinical, radiology and laboratory data were investigated. These data included: age, sex, cause of trauma, GCS at the time of admission, pupil reaction to light, Rotterdam computer tomography (CT) score, hospitalization length, anemia during admission, and high blood sugar during admission. All patients were managed in accordance with the advanced trauma life support protocol for severe head injury where mass lesions are discharged with surgery and all unconscious patients with GCS≤8 are intubated and underwent mechanical ventilation [19].
All patients underwent CT scanning at the time of admission. The CT scans were classified by the main author retrospectively based on the Rotterdam classification system [20]. The clinical outcomes at the time of discharge from the hospital were evaluated using the Glasgow outcome scale (GOS) [7]. This scale grades the outcomes as 5= good recovery; 4= moderate disability; 3= severe disability; 2= persistent vegetative; and 1= death. The data was analyzed using SPSS software, version 23 (SPSS Inc. Chicago, Illinois). Descriptive statistics were reported as median (range) for continuous variables and frequency (percentage) for discrete variables. We used the Chi-Square test or Fisher's exact test to evaluate the difference between ratios. The student T-test was used to evaluate continuous variables. Binary logistic regression analysis was used to evaluate the independent relationship between different variables and clinical results. P<0.05 was considered statistically significant.
Results
In this study, 374 children with moderate to severe TBI were evaluated, of whom 197 (52.7%) were boys and 177 (47.3%) were girls. Their mean age during injury was 7.37±3.11 years. The baseline characteristics of patients are shown in tables 1 and 2.
The univariate regression analysis showed that the GCS score, pupillary light reflex, the Rotterdam CT score, anemia during admission, and high blood sugar during admission were associated with adverse outcomes of TBI in children (P<0.05). Multiple regression analysis results showed the GCS score (OR=3.2; 95% CI: 1.78-5.24; P<0.001), pupillary light reflex (OR=1.97; 95% CI: 1.34-2.99; P=0.024), and the Rotterdam CT score (OR=2.61; 95% CI: 1.72-4.13; P=0.020) had a relationship with clinical outcomes.
Conclusion
The GCS score, pupillary light reflex, and the Rotterdam CT score can predict adverse clinical outcomes in children with moderate to severe TBI. The results of this study can be used to improve the management of these patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethics committee of Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1399.248).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Methodology, supervision: Ehsan Alimohammadi and Seyed Reza Bagheri Bavandpouri; Data collection: Sahel Asadzade and Bita Shokri; Initial draft preparation: Bita Shokri and Ehsan Alimohammadi; Conceptualization, investigation, editing & review: All authors.
Conflicts of interest
The authors declare no conflict of interest.
References
- Appavu B, Foldes ST, Adelson PD. Clinical trials for pediatric traumatic brain injury: Definition of insanity? Journal of Neurosurgery Pediatrics. 2019; 23(6):661-9. [DOI:10.3171/2019.2.PEDS18384] [PMID]
- Araki T, Yokota H, Morita A. Pediatric traumatic brain injury: Characteristic features, diagnosis, and management. Neurologia Medico-Chirurgica. 2017; 57(2):82-93. [DOI:10.2176/nmc.ra.2016-0191] [PMID]
- El-Menyar A, Consunji R, Al-Thani H, Mekkodathil A, Jabbour G, Alyafei KA. Pediatric traumatic brain injury: A 5-year descriptive study from the National Trauma Center in Qatar. World Journal of Emergency Surgery : WJES. 2017; 12:48. [DOI:10.1186/s13017-017-0159-9] [PMID]
- Heneghan JA, Bell MJ. Outcome measures for pediatric traumatic brain injury: Comparing Established and Novel Tests. Pediatric Critical Care Medicine : A Journal of The Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2018; 19(11):1086-7. [DOI:10.1097/PCC.0000000000001731] [PMID]
- Hwang SY, Ong JW, Ng ZM, Foo CY, Chua SZ, Sri D, et al. Long-term outcomes in children with moderate to severe traumatic brain injury: A single-centre retrospective study. Brain Injury. 2019; 33(11):1420-4. [DOI:10.1080/02699052.2019.1641625] [PMID]
- Chiaretti A, Piastra M, Pulitano S, Pietrini D, De Rosa G, Barbaro R, et al. Prognostic factors and outcome of children with severe head injury: An 8-year experience. Child’s Nervous System: ChNS : Official Journal of The International Society for Pediatric Neurosurgery. 2002; 18(3-4):129-36. [DOI:10.1007/s00381-002-0558-3] [PMID]
- Wilson JL, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: Guidelines for their use. Journal of Neurotrauma. 1998; 15(8):573-85. [DOI:10.1089/neu.1998.15.573] [PMID]
- Teasdale GM, Pettigrew LE, Wilson JT, Murray G, Jennett B. Analyzing outcome of treatment of severe head injury: A review and update on advancing the use of the Glasgow Outcome Scale. Journal of Neurotrauma. 1998; 15(8):587-97. [DOI:10.1089/neu.1998.15.587] [PMID]
- Nelson DW, Nyström H, MacCallum RM, Thornquist B, Lilja A, Bellander BM, et al. Extended analysis of early computed tomography scans of traumatic brain injured patients and relations to outcome. Journal of Neurotrauma. 2010; 27(1):51-64. [DOI:10.1089/neu.2009.0986] [PMID]
- Yamagami K, Kurogi R, Kurogi A, Nishimura K, Onozuka D, Ren N, et al. The influence of age on the outcomes of traumatic brain injury: Findings from a Japanese Nationwide Survey (J-ASPECT Study-Traumatic Brain Injury). World Neurosurgery. 2019; 130:e26-46. [PMID]
- Keenan HT, Bratton SL. Epidemiology and outcomes of pediatric traumatic brain injury. Developmental Neuroscience. 2006; 28(4-5):256-63. [DOI:10.1159/000094152] [PMID]
- Maas AI, Hukkelhoven CW, Marshall LF, Steyerberg EW. Prediction of outcome in traumatic brain injury with computed tomographic characteristics: A comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery. 2005; 57(6):1173-82. [DOI:10.1227/01.NEU.0000186013.63046.6B] [PMID]
- Babikian T, Merkley T, Savage RC, Giza CC, Levin H. Chronic aspects of pediatric traumatic brain injury: Review of the literature. Journal of Neurotrauma. 2015; 32(23):1849-60. [DOI:10.1089/neu.2015.3971] [PMID]
- Giza CC, Mink RB, Madikians A. Pediatric traumatic brain injury: Not just little adults. Current Opinion in Critical Care. 2007; 13(2):143-52. [DOI:10.1097/MCC.0b013e32808255dc] [PMID]
- Fay GC, Jaffe KM, Polissar NL, Liao S, J’May BR, Martin KM. Outcome of pediatric traumatic brain injury at three years: A cohort study. Archives of Physical Medicine and Rehabilitation. 1994; 75(7):733-41. [DOI:10.1016/0003-9993(94)90127-9] [PMID]
- Howard I, Joseph JG, Natale JE. Pediatric traumatic brain injury. Ethnicity & Disease. 2005; 15:51-6.
- Bigler ED, Abildskov TJ, Petrie J, Farrer TJ, Dennis M, Simic N, et al. Heterogeneity of brain lesions in pediatric traumatic brain injury. Neuropsychology. 2013; 27(4):438-51. [DOI:10.1037/a0032837] [PMID]
- McCauley SR, Wilde EA, Anderson VA, Bedell G, Beers SR, Campbell TF, et al. Recommendations for the use of common outcome measures in pediatric traumatic brain injury research. Journal of Neurotrauma. 2012; 29(4):678-705. [DOI:10.1089/neu.2011.1838] [PMID]
- Elf K, Nilsson P, Enblad P. Outcome after traumatic brain injury improved by an organized secondary insult program and standardized neurointensive care. Critical Care Medicine. 2002; 30(9):2129-34. [DOI:10.1097/00003246-200209000-00029] [PMID]
- Liesemer K, Riva-Cambrin J, Bennett KS, Bratton SL, Tran H, Metzger RR, et al. Use of Rotterdam CT scores for mortality risk stratification in children with traumatic brain injury. Pediatric Critical Care Medicine. 2014; 15(6):554-62. [DOI:10.1097/PCC.0000000000000150] [PMID]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974; 2(7872):81-4. [PMID]
- Fischer J, Mathieson C. The history of the Glasgow Coma Scale: Implications for practice. Critical Care Nursing Quarterly. 2001; 23(4):52-8. [DOI:10.1097/00002727-200102000-00005] [PMID]
- Gennarelli TA, Champion HR, Copes WS, Sacco WJ. Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. The Journal of Trauma. 1994; 37(6):962-8. [DOI:10.1097/00005373-199412000-00016] [PMID]
- Deepika A, Prabhuraj AR, Saikia A, Shukla D. Comparison of predictability of Marshall and Rotterdam CT scan scoring system in determining early mortality after traumatic brain injury. Acta Neurochirurgica. 2015; 157(11):2033-8. [DOI:10.1007/s00701-015-2575-5] [PMID]
- Kan CH, Saffari M, Khoo TH. Prognostic factors of severe traumatic brain injury outcome in children aged 2-16 years at a major Neurosurgical Referral Centre. Malaysian Journal of Medical Sciences. 2009; 16(4):25-33. [PMID]
- Levin HS, Aldrich EF, Saydjari C, Eisenberg HM, Foulkes MA, Bellefleur M, et al. Severe head injury in children: Experience of the Traumatic Coma Data Bank. Neurosurgery. 1992; 31(3):435-44. [DOI:10.1227/00006123-199209000-00008] [PMID]
- Suresh H, Praharaj S, Indira Devi B, Shukla D, Sastry Kolluri V. Prognosis in children with head injury: An analysis of 340 patients. Neurology India. 2003; 51(1):16-8. [PMID]
Review Paper: Applicable |
Subject:
Special
Received: 2023/07/17 | Accepted: 2023/11/22 | Published: 2024/06/30
Received: 2023/07/17 | Accepted: 2023/11/22 | Published: 2024/06/30
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









