Volume 34, Issue 4 (12-2025)
JGUMS 2025, 34(4): 334-345 |
Back to browse issues page
Research code: 2579
Ethics code: IR.GUMS.REC.1401.050
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ashoobi M T, Musa Zade M, Ebrahimian-Jektaji R, Bolouki M. Investigating the clinical outcome of emergency surgeries and related factors in patients. JGUMS 2025; 34 (4) :334-345
URL: http://journal.gums.ac.ir/article-1-2808-en.html
URL: http://journal.gums.ac.ir/article-1-2808-en.html
1- Department of Surgery, School of Medicine, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Surgery, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Surgery, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 3732 kb]
(74 Downloads)
| Abstract (HTML) (562 Views)
Full-Text: (54 Views)
Introduction
Surgical care is essential for managing a wide spectrum of diseases, with over 234 million procedures performed annually worldwide. In low-and middle-income countries (LMICs), more than 60% of surgeries are emergencies, yet nearly two billion people lack access to essential and emergency surgical services. Surgeries are classified as elective, required, or emergency, with urgent procedures, such as appendectomy or trauma care, being life-saving [1]. Trauma, including road traffic accidents, burns, poisoning, and firearm-related injuries, accounts for 10% of global mortality, with 90% occurring in LMICs. Annually, more than five million people die from injuries, including one million from road traffic accidents, which are the leading cause of injury-related deaths [2]. In Iran, traffic accidents result in approximately 24 000 deaths each year [3].
General surgical emergencies include acute abdominal conditions, bowel obstruction, appendicitis, biliary disease, and infectious abscesses. Surgeries are further categorized as minor, such as biopsies or lesion removal, or major, involving entry into body cavities or amputations [3]. In recent decades, minimally invasive and laparoscopic techniques have expanded, offering significant benefits to patients [4]. However, complications remain a concern, ranging from minor risks (grade i) to death (grade v).
Systematic data sources, such as hospital episode statistics, provide valuable insights into hospital performance, healthcare equity, and policy development [5]. Given the critical role of emergency surgery, continuous evaluation of trends and outcomes is essential.
Methods
This study included patients admitted to the Emergency General Surgery Department of Pour-Sina Hospital, Rasht City, Iran, between 2020 and 2021. Patients were recruited using availability sampling from those undergoing emergency surgical procedures. To maintain consistency, individuals aged 18< years were excluded.
We collected a wide range of information, starting with demographic data, such as age and sex, and extending to details about the surgery itself, including the type of operation and its level of invasiveness. Postoperative outcomes were also carefully recorded, focusing on complications, length of hospital stay, and final surgical results. For clarity, complications were classified into five stages: Minor issues manageable with simple treatment (stage I), moderate complications requiring additional care, such as antibiotics or drainage (stage II), major problems requiring repeat surgery or ICU admission (stage III), life-threatening conditions requiring urgent intervention (stage IV), and catastrophic outcomes leading to disability or death (stage V).
The data were analyzed using descriptive and inferential statistics. A combination of averages, variability measures, tables, and charts was used to describe the findings, while chi-square tests explored relationships between surgical types and other factors. A significance level of 0.05 was applied, and all analyses were performed using IBM SPSS software, version 24 (USA). The sample size was estimated using Cochran’s formula, with a 71% prevalence of trauma-related emergencies reported by Ibrahim et al. [6].
Results
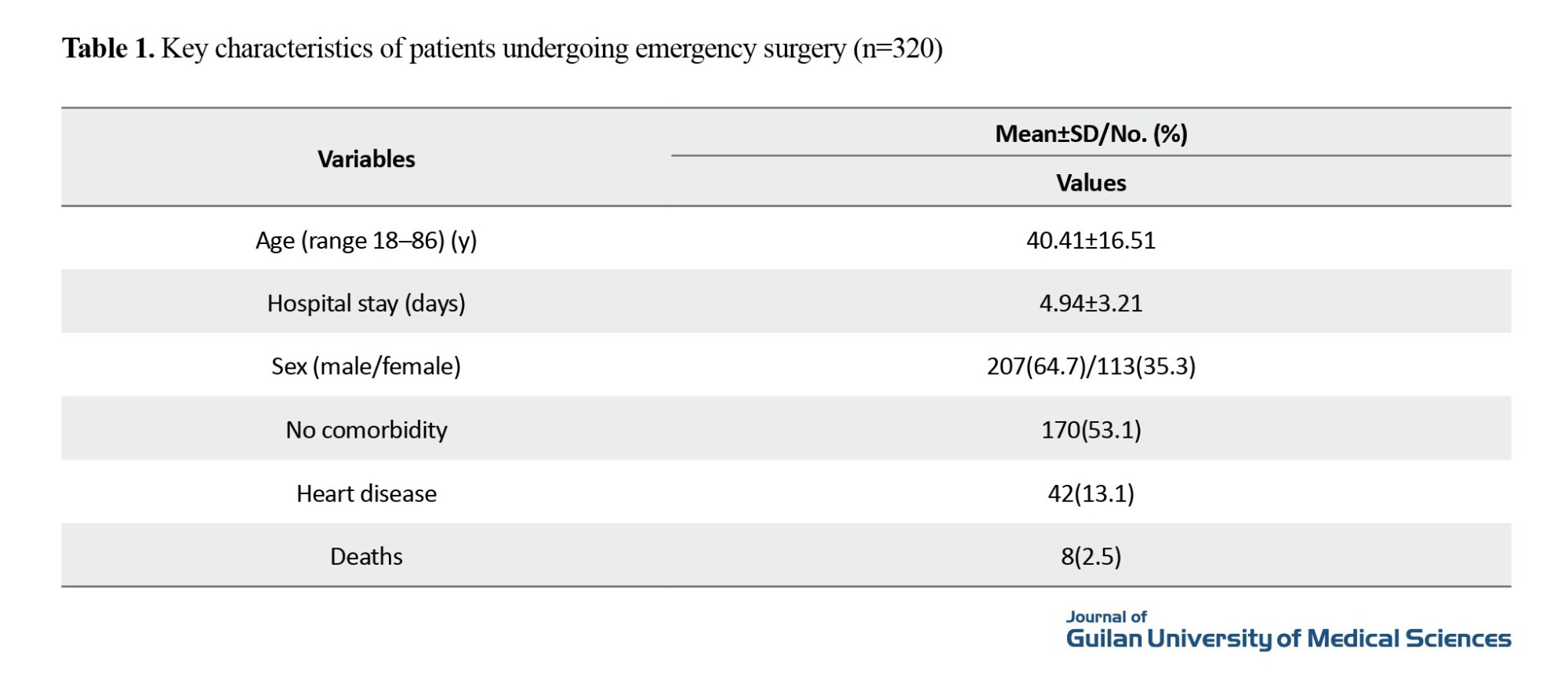
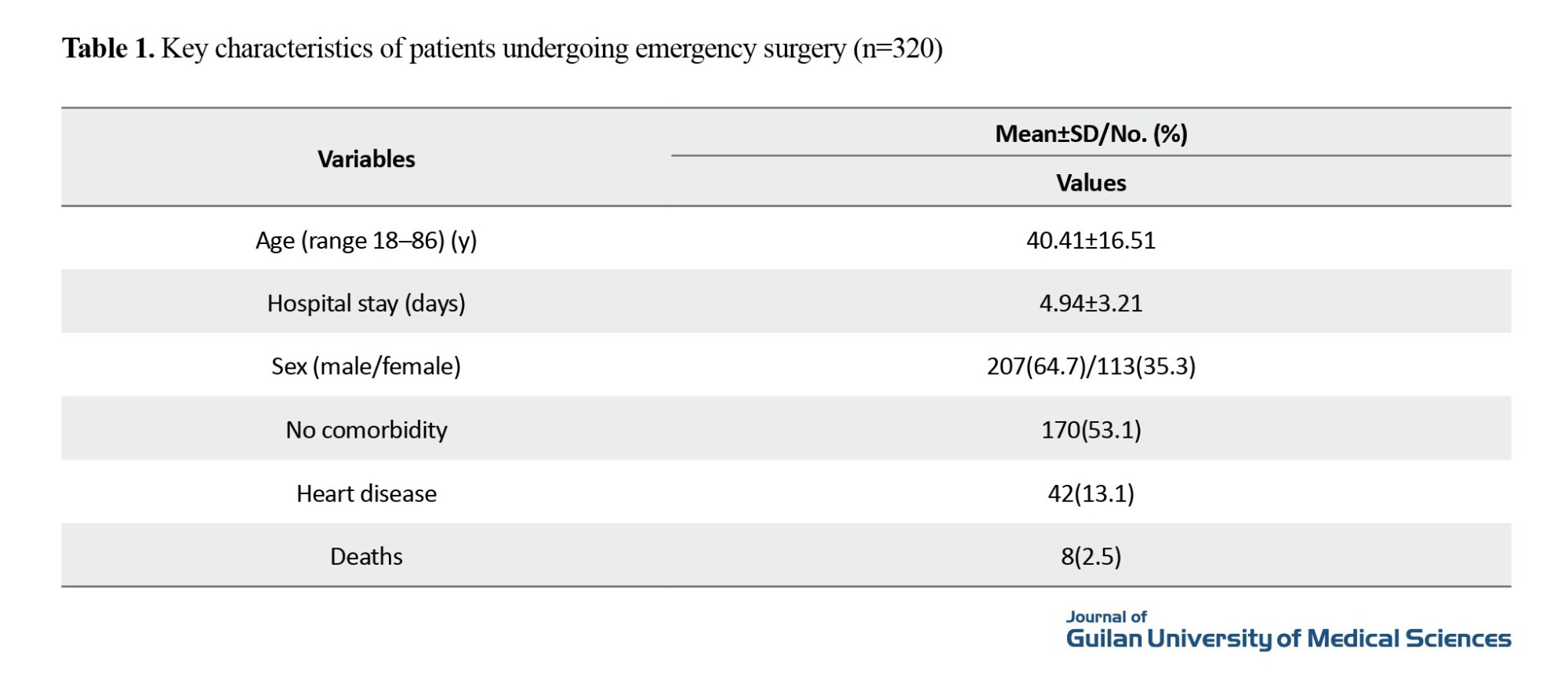
A total of 320 patients undergoing emergency surgery were evaluated. The age of patients ranged from 18 to 86 years, with a mean of 40.41±16.51 years. The average duration of hospitalization was 4.94±3.21 days. Of the participants, 207(64.7%) were male and 113(35.3%) female. More than half of the patients (53.1%) had no significant comorbidities, and the most frequent underlying disease was heart disease (13.1%).
The majority of emergency procedures were abdominal, particularly appendectomies, followed by trauma-related surgery. Most operations were classified as major and invasive. Postoperative complications were generally mild to moderate, with grade I and II complications being the most common. Despite this, eight deaths were recorded, while the remaining patients were discharged after recovery.
Statistical analysis indicated a significant relationship between the type of surgery and hospital stay (P=0.000). Furthermore, chi-square testing revealed a strong association between surgical complications and procedure type. Patients with trauma had the highest incidence of severe outcomes, including Grade V mortality, while appendectomy patients most often experienced minor complications (grade I) (Table 1).
Conclusion
Non-traumatic emergency surgeries remain common, with gastrointestinal operations, such as appendectomy, colectomy, and hernia repair at the forefront. Given their burden on healthcare systems, identifying risk factors for complications and prolonged hospitalization is critical. Our findings emphasize that the type of surgery strongly influences outcomes, underscoring the need for tailored perioperative strategies.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1401.050).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Data analysis, and interpretation of data: Mohammad Taghi Ashoobi and Ramin Ebrahimian-Jektaji; Drafting of the manuscript: Mehdi Musa Zade, Mohammad Taghi Ashoobi, Ramin Ebrahimian-Jektaji; Critical revision of the manuscript: Mehdi Musa Zade, Mohammad Taghi Ashoobi, Motahareh Bolouki; Satatical analysis: Mehdi Musa Zade, Mohammad Taghi Ashoobi, Ramin Ebrahimian-Jektaji; Obtained funding: Mehdi Musa Zade and Ramin Ebrahimian-Jektaji; Administrative, technical, or material support: Mehdi Musa Zade, Mohammad Taghi Ashoobi; Study supervision: Mehdo Musa Zade and Mohammad Taghi Ashoobi; Conceptualization, study design and final approval: All Authors.
Conflicts of interest
The authors declared no conflicts of interest.
Acknowledgments
The authors thank Guilan University of Medical Sciences for their assistance and guidance in this study.
Surgical care is essential for managing a wide spectrum of diseases, with over 234 million procedures performed annually worldwide. In low-and middle-income countries (LMICs), more than 60% of surgeries are emergencies, yet nearly two billion people lack access to essential and emergency surgical services. Surgeries are classified as elective, required, or emergency, with urgent procedures, such as appendectomy or trauma care, being life-saving [1]. Trauma, including road traffic accidents, burns, poisoning, and firearm-related injuries, accounts for 10% of global mortality, with 90% occurring in LMICs. Annually, more than five million people die from injuries, including one million from road traffic accidents, which are the leading cause of injury-related deaths [2]. In Iran, traffic accidents result in approximately 24 000 deaths each year [3].
General surgical emergencies include acute abdominal conditions, bowel obstruction, appendicitis, biliary disease, and infectious abscesses. Surgeries are further categorized as minor, such as biopsies or lesion removal, or major, involving entry into body cavities or amputations [3]. In recent decades, minimally invasive and laparoscopic techniques have expanded, offering significant benefits to patients [4]. However, complications remain a concern, ranging from minor risks (grade i) to death (grade v).
Systematic data sources, such as hospital episode statistics, provide valuable insights into hospital performance, healthcare equity, and policy development [5]. Given the critical role of emergency surgery, continuous evaluation of trends and outcomes is essential.
Methods
This study included patients admitted to the Emergency General Surgery Department of Pour-Sina Hospital, Rasht City, Iran, between 2020 and 2021. Patients were recruited using availability sampling from those undergoing emergency surgical procedures. To maintain consistency, individuals aged 18< years were excluded.
We collected a wide range of information, starting with demographic data, such as age and sex, and extending to details about the surgery itself, including the type of operation and its level of invasiveness. Postoperative outcomes were also carefully recorded, focusing on complications, length of hospital stay, and final surgical results. For clarity, complications were classified into five stages: Minor issues manageable with simple treatment (stage I), moderate complications requiring additional care, such as antibiotics or drainage (stage II), major problems requiring repeat surgery or ICU admission (stage III), life-threatening conditions requiring urgent intervention (stage IV), and catastrophic outcomes leading to disability or death (stage V).
The data were analyzed using descriptive and inferential statistics. A combination of averages, variability measures, tables, and charts was used to describe the findings, while chi-square tests explored relationships between surgical types and other factors. A significance level of 0.05 was applied, and all analyses were performed using IBM SPSS software, version 24 (USA). The sample size was estimated using Cochran’s formula, with a 71% prevalence of trauma-related emergencies reported by Ibrahim et al. [6].
Results
A total of 320 patients undergoing emergency surgery were evaluated. The age of patients ranged from 18 to 86 years, with a mean of 40.41±16.51 years. The average duration of hospitalization was 4.94±3.21 days. Of the participants, 207(64.7%) were male and 113(35.3%) female. More than half of the patients (53.1%) had no significant comorbidities, and the most frequent underlying disease was heart disease (13.1%).
The majority of emergency procedures were abdominal, particularly appendectomies, followed by trauma-related surgery. Most operations were classified as major and invasive. Postoperative complications were generally mild to moderate, with grade I and II complications being the most common. Despite this, eight deaths were recorded, while the remaining patients were discharged after recovery.
Statistical analysis indicated a significant relationship between the type of surgery and hospital stay (P=0.000). Furthermore, chi-square testing revealed a strong association between surgical complications and procedure type. Patients with trauma had the highest incidence of severe outcomes, including Grade V mortality, while appendectomy patients most often experienced minor complications (grade I) (Table 1).
Conclusion
Non-traumatic emergency surgeries remain common, with gastrointestinal operations, such as appendectomy, colectomy, and hernia repair at the forefront. Given their burden on healthcare systems, identifying risk factors for complications and prolonged hospitalization is critical. Our findings emphasize that the type of surgery strongly influences outcomes, underscoring the need for tailored perioperative strategies.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1401.050).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Data analysis, and interpretation of data: Mohammad Taghi Ashoobi and Ramin Ebrahimian-Jektaji; Drafting of the manuscript: Mehdi Musa Zade, Mohammad Taghi Ashoobi, Ramin Ebrahimian-Jektaji; Critical revision of the manuscript: Mehdi Musa Zade, Mohammad Taghi Ashoobi, Motahareh Bolouki; Satatical analysis: Mehdi Musa Zade, Mohammad Taghi Ashoobi, Ramin Ebrahimian-Jektaji; Obtained funding: Mehdi Musa Zade and Ramin Ebrahimian-Jektaji; Administrative, technical, or material support: Mehdi Musa Zade, Mohammad Taghi Ashoobi; Study supervision: Mehdo Musa Zade and Mohammad Taghi Ashoobi; Conceptualization, study design and final approval: All Authors.
Conflicts of interest
The authors declared no conflicts of interest.
Acknowledgments
The authors thank Guilan University of Medical Sciences for their assistance and guidance in this study.
References
- Rose J, Chang DC, Weiser TG, Kassebaum NJ, Bickler SW. The role of surgery in global health: Analysis of United States inpatient procedure frequency by condition using the Global Burden of Disease 2010 framework. Plos One. 2014; 9(2):e89693. [DOI:10.1371/journal.pone.0089693]
- Mogharab V, Ostovar M, Ruszkowski J, Hussain SZM, Shrestha R, Yaqoob U, et al. Global burden of the COVID-19 associated patient-related delay in emergency healthcare: A panel of systematic review and meta-analyses. Globalization and Health. 2022;18(1):58. [DOI:10.1186/s12992-022-00836-2]
- Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, Uribe-Leitz T, et al. Size and distribution of the global volume of surgery in 2012. Bulletin of the World Health Organization. 2016; 94(3):201. [DOI:10.2471/BLT.15.159293]
- Kushner AL, Cherian MN, Noel L, Spiegel DA, Groth S, Etienne C. Addressing the millennium development goals from a surgical perspective: Essential surgery and anesthesia in 8 low-and middle-income countries. Archives of Surgery. 2010; 145(2):154-9. [DOI:10.1001/archsurg.2009.263]
- Birnbaum FA, Neeson C, Solá-Del Valle D. Microinvasive glaucoma surgery: An evidence-based review. Seminars in Ophthalmology. 2021; 36(8):772-86. [DOI:10.1080/08820538.2021.1903513]
- Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bulletin of the World Health Organization. 2007; 85(9):695-702. [DOI:10.2471/BLT.06.037184]
- Søreide K. Epidemiology of major trauma. British Journal of Surgery. 2009; 96(7):697-8. [DOI:10.1002/bjs.6643]
- Chitturi MV, Ooms AW, Bill AR, Noyce DA. Injury outcomes and costs for cross-median and median barrier crashes. Journal of Safety Research. 2011; 42(2):87-92. [DOI:10.1016/j.jsr.2011.01.006]
- Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet Journal. 2015; 385(9963):117-71. [DOI:10.1016/S0140-6736(14)61682-2]
- Kashani AT, Shariat-Mohaymany A, Ranjbari A. Analysis of factors associated with traffic injury severity on rural roads in Iran. Journal of Injury & Violence Research. 2012; 4(1):36-41. [DOI:10.5249/jivr.v4i1.67] [PMID]
- Bickler S, Ozgediz D, Gosselin R, Weiser T, Spiegel D, Hsia R, et al. Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World Journal of Surgery. 2010; 34:374-80. [DOI:10.1007/s00268-009-0261-6]
- Fingar KR, Stocks C, Weiss AJ, Steiner CA. Most frequent operating room procedures performed in U.S. hospitals, 2003–2012. 2014 Dec. In: Healthcare Cost and Utilization Project (Hcup) Statistical Brief. Rockville (MD): Agency for healthcare research and quality (US). Bordeaux: HCUP; 2006. [Link]
- Richards MK, McAteer JP, Drake FT, Goldin AB, Khandelwal S, Gow KW. A national review of the frequency of minimally invasive surgery among general surgery residents: Assessment of ACGME case logs during 2 decades of general surgery resident training. JAMA Surgery. 2015; 150(2):169-72. [DOI:10.1001/jamasurg.2014.1791]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery. 2004; 240(2):205-13. [DOI:10.1097/01.sla.0000133083.54934.ae]
- Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on st-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020; 13(4):e006631. [DOI:10.1161/CIRCOUTCOMES.120.006631]
- Shiekh SI, Harley M, Ghosh RE, Ashworth M, Myles P, Booth HP, et al. Completeness, agreement, and representativeness of ethnicity recording in the United Kingdom’s clinical practice research datalink (CPRD) and linked hospital episode statistics (HES). Population Health Metrics. 2023; 21(1):3. [DOI:10.1186/s12963-023-00302-0]
- Ibrahim NA, Oludara MA, Ajani A, Mustafa I, Balogun R, Idowu O, et al. Non-trauma surgical emergencies in adults: Spectrum, challenges and outcome of care. Annals of Medicine & Surgery. 2015; 4(4):325-30. [DOI:10.1016/j.amsu.2015.09.004]
- Wohlgemut JM, Ramsay G, Jansen JO. The changing face of emergency general surgery: A 20-year analysis of secular trends in demographics, diagnoses, operations, and outcomes. Annals of Surgery. 2020; 271(3):581-9. [DOI:10.1097/SLA.0000000000003066]
- Ward TL, Raybould SJ, Mondal A, Lambert J, Patel B. Predicting the length of stay at admission for emergency general surgery patients a cohort study. Annals of Medicine and Surgery. 2021; 62:127-30. [DOI:10.1016/j.amsu.2021.01.011]
- Lee JY, Lee SH, Jung MJ, Lee JG. Perioperative risk factors for in-hospital mortality after emergency gastrointestinal surgery. Medicine. 2016; 95(35):e4530. [DOI:10.1097/MD.0000000000004530]
- Watt DG, Wilson MS, Shapter OC, Patil P. 30-Day and 1-year mortality in emergency general surgery laparotomies: An area of concern and need for improvement? European Journal of Trauma and Emergency Surgery. 2015; 41(4):369-74. [DOI:10.1007/s00068-014-0450-3]
- Merani S, Payne J, Padwal RS, Hudson D, Widder SL, Khadaroo RG. Predictors of in-hospital mortality and complications in very elderly patients undergoing emergency surgery. World Journal of Emergency Surgery. 2014; 9:43. [DOI:10.1186/1749-7922-9-43]
- Tribuddharat S, Sathitkarnmanee T, Sappayanon P. Emergency surgery mortality (ESM) score to predict mortality and improve patient care in emergency surgery. Anesthesiology Research and Practice. 2019; 2019:6760470. [DOI:10.1155/2019/6760470]
- Achanta A, Nordestgaard A, Kongkaewpaisan N, Han K, Mendoza A, Saillant N, et al. Most of the variation in length of stay in emergency general surgery is not related to clinical factors of patient care. Journal of Trauma and Acute Care Surgery. 2019; 87(2):408-12. [DOI:10.1097/TA.0000000000002279]
- Hutchings A, Moler Zapata S, O’Neill S, Smart N, Cromwell D, Hinchliffe R, et al. Variation in the rates of emergency surgery amongst emergency admissions to hospital for common acute conditions. BJS Open. 2021; 5(6):zrab094. [DOI:10.1093/bjsopen/zrab094]
- Wirachpisit N, Choovongkomol C, Komonhirun R, Poomhirun P, Ittichaikulthol W. Incidence, risk factors, and complications associated with in-hospital mortality in emergency surgery at Ramathibodi hospital: A retrospective study. Ramathibodi Medical Journal. 2018; 41(2):67-77. [DOI:10.14456/rmj.2018.19]
- Hatchimonji JS, Swendiman RA, Kaufman EJ, Scantling D, Passman JE, Yang W, et al. Multiple complications in emergency surgery: Identifying risk factors for failure-to-rescue. The American Surgeon. 2020; 86(7):787-95. [DOI:10.1177/0003134820934400]
- Ylimartimo AT, Nurkkala J, Koskela M, Lahtinen S, Kaakinen T, Vakkala M, et al. Postoperative complications and outcome after emergency laparotomy: A retrospective study. World Journal of Surgery. 2023; 47(1):119-29. [DOI:10.1007/s00268-022-06783-8]
- Abbott TEF, Fowler AJ, Dobbs TD, Harrison EM, Gillies MA, Pearse RM. Frequency of surgical treatment and related hospital procedures in the UK: A national ecological study using hospital episode statistics. British Journal of Anaesthesia. 2017; 119(2):249-57. [DOI:10.1093/bja/aex137]
Review Paper: Research |
Subject:
General
Received: 2025/08/5 | Accepted: 2025/03/9 | Published: 2026/01/1
Received: 2025/08/5 | Accepted: 2025/03/9 | Published: 2026/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |